Background
Cataract remains the leading cause of visual impairment globally, significantly impacting the quality of life, especially in aging populations. While aging is the primary risk factor, modifiable behaviors such as sleep quality, physical activity (PA), and sedentary behavior (SB) are increasingly recognized for their roles in cataract pathogenesis. Prior studies investigating these factors have provided inconsistent and sometimes contradictory findings, often limited by small sample sizes and unidimensional behavioral measures. There is a pressing need to understand how these daily lifestyle factors individually and collectively influence cataract risk to guide effective prevention strategies.
Study Design and Methods
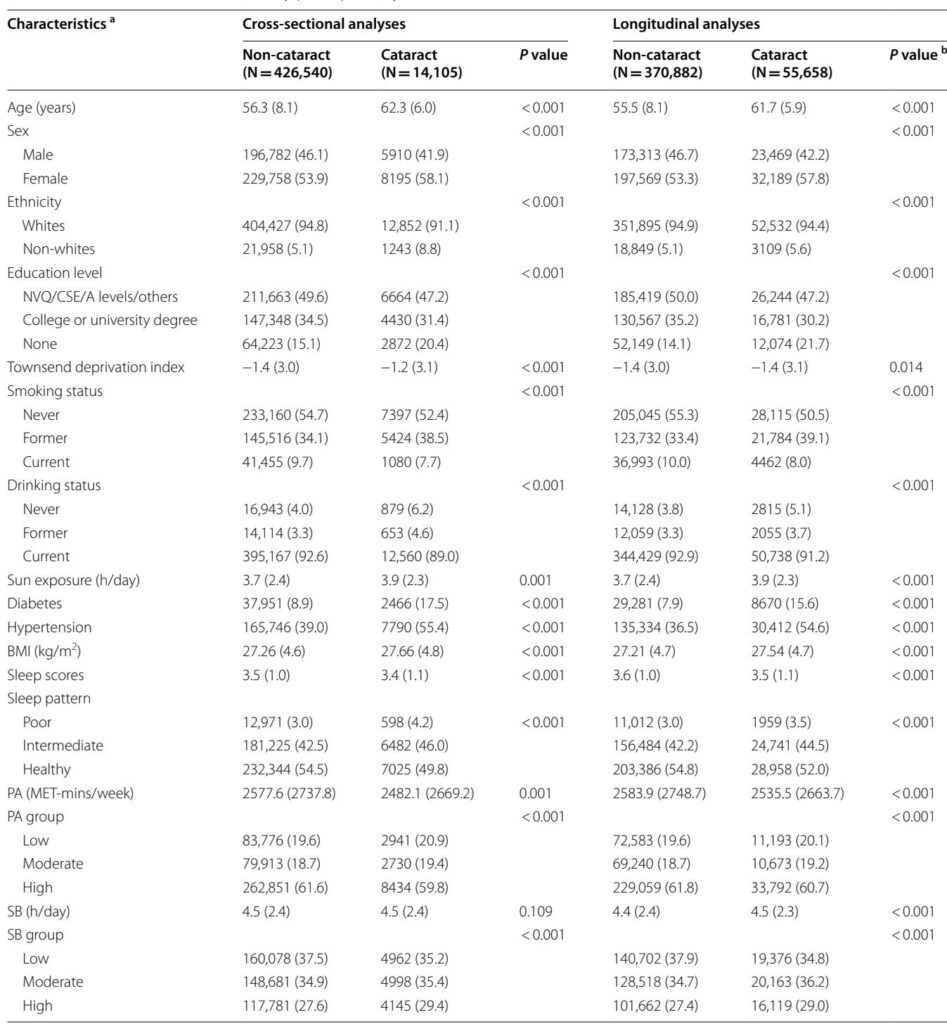
This investigation utilized data from the UK Biobank, a prospective cohort of over 500,000 participants aged 37 to 73 years across the UK. Cross-sectional analyses included 440,645 participants with complete baseline data on sleep, PA, and SB, while longitudinal analyses focused on 426,540 participants free of cataract at baseline and followed up for a mean of 10.8 years.
Cataract cases were ascertained through hospital inpatient records and self-reported data. Sleep quality was evaluated using a composite sleep score covering five dimensions: chronotype, duration, insomnia, snoring, and daytime sleepiness. PA was quantified in metabolic equivalent task (MET)-minutes per week based on walking, moderate, and vigorous activities. SB was assessed by daily hours spent watching television, using computers for non-work purposes, and driving. Participants were stratified into categories based on healthy cutoffs:
– Sleep: poor, intermediate, healthy
– PA: low (<600 MET-min/week), moderate, high
– SB: low (<4 h/day), moderate (4–5 h/day), high (≥6 h/day)
Multivariable logistic regression and Cox proportional hazards models were employed, adjusting for potential confounders including age, sex, ethnicity, socioeconomic status, education, BMI, smoking, alcohol use, sun exposure, diabetes, and hypertension. Additionally, isotemporal substitution analysis modeled the effect of replacing sedentary time with equal durations of PA or sleep on cataract risk. Subgroup and sensitivity analyses further evaluated robustness and effect modifications.
Key Findings
Independent Associations:
– Poor sleep quality significantly increased cataract risk: cross-sectional odds ratio (OR) 1.35 (95% CI 1.23–1.48), prospective hazard ratio (HR) 1.14 (95% CI 1.08–1.19).
– Low physical activity associated with higher cataract risk: cross-sectional OR 1.06 (95% CI 1.01–1.11), prospective HR 1.05 (95% CI 1.02–1.07).
– High sedentary behavior was independently linked to an increased prospective cataract risk: HR 1.08 (95% CI 1.06–1.11), although cross-sectional associations were borderline.
Dose-response analyses confirmed linear or L-shaped relationships, with lowest risks observed at approximately 5000 MET-min/week of PA and composite high sleep scores. Accelerometer-based measures corroborated these associations.
Joint and Synergistic Effects:
– Combined exposure to poor sleep, low PA, and high SB conferred the greatest risk of cataract development, with cross-sectional OR 1.73 (95% CI 1.37–2.15) and prospective HR 1.37 (95% CI 1.21–1.55) compared to favorable behavior groups.
– Interaction analyses revealed additive and multiplicative effects among these behaviors, emphasizing the importance of considering multiple lifestyle factors simultaneously.
Isotemporal Substitution Model:
– Replacing 1 hour/day of sedentary time with physical activity reduced cataract risk by 1.7%, while substitution with sleep reduced risk by 2.7% in the whole cohort.
– Among individuals sleeping ≤7 hours/day, substitution with sleep yielded greater risk reduction compared to PA, highlighting personalized intervention targets.
Subgroup and Sensitivity Analyses:
– The relationships were consistent across age, sex, and diabetes subgroups, though sleep and SB impacts were more prominent in midlife, and PA effects stronger in males.
– Findings remained robust after adjustments for potential confounders, exclusion of early cases to limit reverse causation, and when using objectively measured movement behaviors.
Expert Commentary
This comprehensive study from the UK Biobank addresses previous uncertainties by leveraging a large, well-characterized cohort with detailed behavioral assessments and long follow-up. The demonstration that sleep quality, physical activity, and sedentary time independently and jointly influence cataract risk advances clinical understanding and provides a foundation for integrated lifestyle interventions.
The use of a composite sleep score recognizes the multifaceted nature of sleep health beyond duration alone and aligns with growing evidence linking circadian and inflammatory pathways to ocular tissue homeostasis and cataractogenesis. Biological plausibility is supported by the known role of oxidative stress and systemic inflammation in lens opacity development.
The isotemporal substitution analysis offers practical insights: encouraging moderate-to-vigorous physical activity and optimizing sleep duration especially in insufficient sleepers may offer additive protective benefits. Given the interaction among behaviors, multidomain intervention strategies are likely more impactful than targeting any single behavior.
Limitations include reliance on self-reported behavioral data for primary analyses, potential residual confounding, and cataract ascertainment based on health records which may underestimate true incidence. The predominantly White UK-based cohort aged 37–73 years may limit generalizability to other ethnic or younger populations.
Overall, this investigation fills a critical knowledge gap by elucidating how modifiable lifestyle factors converge to influence cataract risk, underscoring the importance of holistic preventive strategies in ophthalmic public health.
Conclusions
Poor sleep quality, low physical activity, and high sedentary behavior independently increase the risk of cataract development, and their combined presence further elevates this risk. Substituting sedentary time with physical activity or improving sleep duration effectively reduces cataract incidence. Public health interventions aiming to encourage at least 600 MET-min/week of physical activity, limit sedentary time to under 6 hours daily, and promote 7–8 hours of quality sleep could significantly mitigate cataract burden. These findings highlight the beneficial impact of integrated lifestyle modification on eye health, offering actionable targets for cataract prevention.