Background
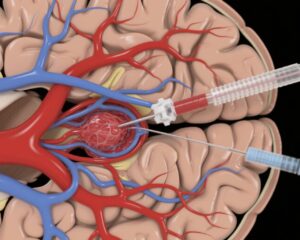
Ischemic stroke in patients with nonvalvular atrial fibrillation (AF) poses a high risk of recurrent thromboembolic events. Direct oral anticoagulants (DOACs) have transformed stroke prevention in AF due to better safety and efficacy profiles compared to vitamin K antagonists. Early initiation of DOACs after ischemic stroke has demonstrated benefits in preventing recurrence while being relatively safe concerning bleeding complications. However, the timing of anticoagulation initiation after acute stroke remains a clinical challenge, particularly when patients have undergone reperfusion therapy such as intravenous thrombolysis (IVT) and endovascular treatment (EVT). These reperfusion modalities, essential for restoring cerebral blood flow, carry their own risk profiles, including hemorrhagic transformation of infarcts.
Understanding whether prior acute reperfusion therapy modifies the risks and benefits of early versus delayed DOAC initiation is critical to optimize stroke management. The randomized controlled ELAN (Early versus Late Initiation of Direct Oral Anticoagulants in post-Ischemic Stroke patients with Atrial Fibrillation) trial has previously established the safety of early DOAC initiation post-ischemic stroke. This prespecified subanalysis aims to explore if prior reperfusion strategy influences clinical outcomes related to the timing of DOAC initiation.
Study Design
This post hoc analysis included 1973 patients (98% of the original ELAN trial population) with acute ischemic stroke and nonvalvular AF, across multiple centers, randomized to early versus late DOAC initiation. Patients were grouped by prior reperfusion therapy received before randomization: no reperfusion, IVT alone, EVT alone, or IVT combined with EVT.
The primary composite outcome assessed within 30 days included recurrent ischemic stroke, symptomatic intracranial hemorrhage, major extracranial bleeding, systemic embolism, or vascular death. Logistic regression models adjusted for important confounders (age, hypertension, infarct characteristics, pre-stroke disability, stroke severity assessed by NIH Stroke Scale [NIHSS], and hemorrhagic transformation) examined the interaction between reperfusion strategy and timing of anticoagulation initiation.
Key Findings
Demographics showed a median age of 77 years and nearly equal gender distribution (46% female). The distribution by reperfusion therapy was: 51% no reperfusion, 26% IVT, 10% EVT, and 13% combined IVT+EVT.
No statistically significant interaction was identified between prior reperfusion treatment and timing of DOAC initiation for the composite or individual outcomes. Numerically, early DOAC initiation tended toward lower event rates in patients without reperfusion therapy (3.3% vs. 4.8%), with EVT alone (1.2% vs. 6.4%), and EVT combined with IVT (2.4% vs. 3.3%). For patients treated with IVT alone, rates of adverse events were slightly higher with early DOAC (3% vs. 2%), but this was not statistically significant.
Adjusted odds ratios suggested no modification effect, supporting that the timing of DOAC initiation after an ischemic stroke is safe and effective regardless of prior reperfusion strategy. The data imply that clinicians might consider early DOAC initiation without deferring due to a history of IVT or EVT.
Expert Commentary
The ELAN trial subanalysis provides important evidence to guide anticoagulation timing decisions in complex stroke care scenarios. Previous concerns about hemorrhagic risk after reperfusion therapies have often led to delayed anticoagulation in clinical practice. These findings mitigate that apprehension by demonstrating no interaction effect of reperfusion on outcomes with early DOAC start.
Limitations of this analysis include its post hoc nature and the relatively small subgroup sizes for EVT and combined EVT+IVT cohorts, which could limit statistical power for interaction detection. Further studies could explore longer-term outcomes and different stroke severities. Nonetheless, this study aligns with accumulating evidence supporting early anticoagulation initiation as a safe approach in AF-related ischemic stroke.
Conclusion
This prespecified subanalysis of the ELAN trial confirms that prior reperfusion therapy does not modify the effect of early versus late DOAC initiation on key clinical outcomes in patients with atrial fibrillation and acute ischemic stroke. Early anticoagulation remains a safe and beneficial strategy across different reperfusion modalities, encouraging prompt secondary stroke prevention without additional delay in this patient population.
References
Wouters A, Demeestere J, Rossel JB, Devroye A, Desfontaines P, Vanacker P, Hemelsoet D, Yperzeele L, Rutgers MP, Peeters A, Vynckier J, Yoshimoto T, Tanaka K, Vehoff J, Matsuzono K, Kulyk C, Sibolt G, Slade P, Salerno A, Kunieda T, Hakim A, Rohner R, Abend S, Goeldlin M, Dawson J, Fischer U, Lemmens R; ELAN Investigators. Prior Reperfusion Strategy Does Not Modify Outcome in Early Versus Late Start of Anticoagulants in Patients With Ischemic Stroke: Prespecified Subanalysis of the Randomized Controlled ELAN Trial. Stroke. 2025 Aug;56(8):2000-2008. doi: 10.1161/STROKEAHA.125.050646. Epub 2025 May 22. PMID: 40402090.