Introduction
Obesity poses a significant global health challenge, with more than two billion adults affected worldwide and projections indicating continued growth in prevalence. It substantially elevates risks of morbidity and mortality and exerts heavy economic burdens. Traditional obesity management strategies—including diet, exercise, and behavioral therapy—are effective at the individual level but face limitations in scalability, accessibility, and maintaining long-term adherence. Digital health modalities, namely electronic health (e-health) and mobile health (m-health), leverage technology to overcome these barriers by providing personalized, scalable, and continuous support for lifestyle modifications. This systematic review and meta-analysis collates evidence from randomized controlled trials (RCTs) to evaluate the impact of digital health interventions on anthropometric measures and lifestyle behaviors in overweight and obese adults.
Study Design and Methods
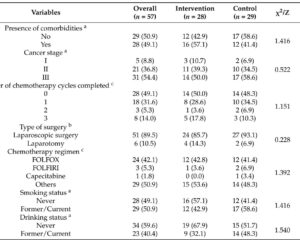
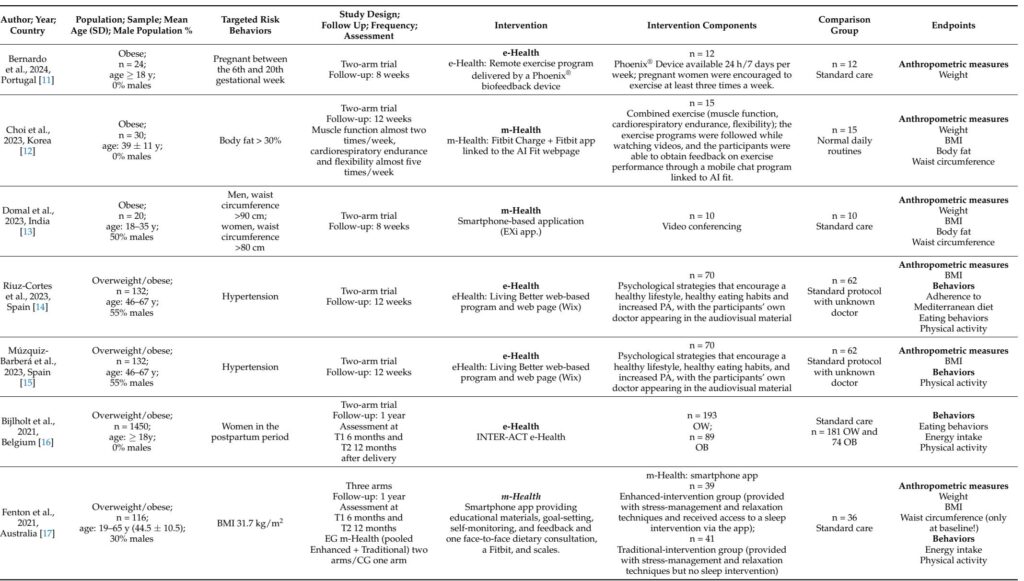
A comprehensive literature search was conducted through Medline, Scopus, and Web of Science up to October 4, 2024, identifying 22 RCTs enrolling overweight or obese adults (BMI≥25 kg/m²). Included studies evaluated diverse digital interventions—ranging from biofeedback devices, smartphone apps, e-coaching, text messaging, to web-based platforms—versus standard care or no intervention. Outcomes assessed comprised anthropometric indicators (BMI, weight, waist circumference, body-fat percentage) and lifestyle behaviors (physical activity, energy intake, eating patterns). Quality was appraised via the Cochrane Risk of Bias Tool (RoB 2), and data synthesis used fixed- or random-effects meta-analyses depending on heterogeneity, with GRADE applied to evaluate evidence certainty.
Key Findings
The meta-analysis revealed a statistically significant but modest reduction in waist circumference (weighted mean difference [WMD]: -1.77 cm; 95% CI: -3.10 to -0.44; p=0.009), an important independent predictor of cardiometabolic risk. Other anthropometric outcomes, including BMI (WMD: -0.43 kg/m²; p=0.247), body weight (WMD: 0.42 kg; p=0.341), and body-fat percentage (trend toward reduction: WMD: -0.79%; p=0.068), did not reach significance. Lifestyle behaviors such as physical activity, energy intake, and eating behaviors showed no significant overall changes, though subgroup analyses indicated Generation X participants were more responsive to digital interventions.
High heterogeneity (I² >80%) across most outcomes underscored variability related to participant populations, intervention types, duration, and methodological quality. Sensitivity analyses excluding high-risk-of-bias studies upheld the main findings, indicating robustness. No significant publication bias was identified.
Expert Commentary
The isolated significant effect on waist circumference is clinically meaningful given its role as a predictor of cardiovascular and metabolic disease independent of BMI changes. Digital health interventions offer continuous monitoring and feedback that may influence abdominal adiposity more effectively than broader weight metrics. The lack of significant effects on weight, BMI, and behavior likely reflects heterogeneous interventions, short follow-up durations, varying adherence, and the challenges of behavioral change via digital platforms alone.
Variation in digital literacy and engagement across populations, especially older adults, and the diverse technological modalities—ranging in complexity and interactivity—further contribute to inconsistent outcomes. The evidence suggests that digital therapies function best as supplements integrated within comprehensive obesity management programs, rather than standalone treatments. Future digital interventions should incorporate personalized adaptive algorithms and clinician oversight to enhance effectiveness and adherence.
The moderate certainty of evidence for waist circumference reduction and low to very low certainty for behavioral outcomes highlights the need for high-quality, long-term trials evaluating standardized, multifaceted digital interventions tailored to user profiles.
Conclusions
Digital health interventions demonstrate promise in reducing waist circumference among overweight and obese adults, representing a meaningful step forward in obesity care scalability. However, their effects on weight, BMI, and lifestyle behaviors remain inconclusive amid substantial heterogeneity and methodological limitations. These findings advocate for deploying digital strategies as adjuncts within integrated obesity treatment frameworks, emphasizing personalization, digital literacy support, and sustained engagement. Advanced research delineating optimal intervention components, durations, and target populations is imperative to fully realize the potential of e-health and m-health in comprehensive obesity management.
Reference
Chiavarini M, Giacchetta I, Rosignoli P, Fabiani R. E-Health and M-Health in Obesity Management: A Systematic Review and Meta-Analysis of RCTs. Nutrients. 2025 Jul 1;17(13):2200. doi: 10.3390/nu17132200. PMID: 40647304; PMCID: PMC12251417.