Highlight
– Single-cell and spatial transcriptomics identify a previously unrecognized PRR4⁺CST3⁺WFDC2⁻ seromucous acinar population that is selectively depleted in Sjögren’s disease (SjD).
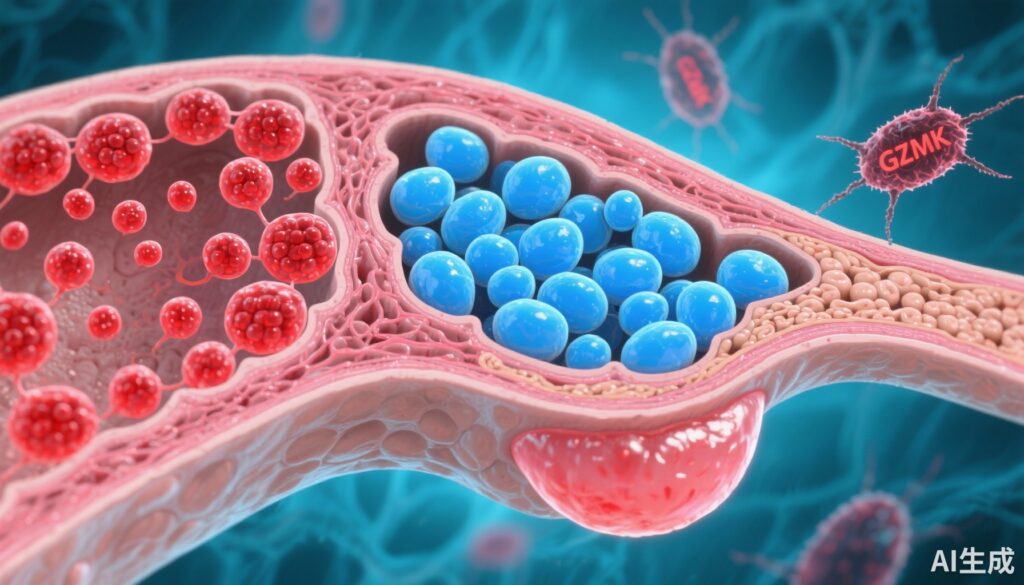
– GZMK⁺CD8⁺ T cells accumulate with disease severity, show a cytotoxic yet sub-lytic program, and spatially co-localize with immune-engaged epithelial cells.
– Functional assays indicate GZMK impairs mitochondrial integrity and triggers interferon signaling in epithelial cells — linking targeted epithelial injury to type I interferon responses and suggesting new therapeutic targets.
Background: clinical context and unmet need
Sjögren’s disease (SjD) is a chronic systemic autoimmune disorder that preferentially targets exocrine glands, notably the salivary and lacrimal glands, causing sicca symptoms, fatigue, and systemic manifestations. Disease heterogeneity — ranging from focal lymphocytic infiltration with preserved gland function to widespread epithelial damage with systemic involvement — complicates diagnosis and therapy. Current treatments are largely symptomatic; disease-modifying strategies remain limited by incomplete understanding of the target cells, pathogenic immune effectors, and mechanisms driving glandular dysfunction.
Single-cell and spatial profiling technologies provide an opportunity to map the tissue microenvironment at cellular resolution and to link cellular phenotypes to clinical endotypes. The study by Pranzatelli et al. (Ann Rheum Dis. 2025) uses these tools combined with patient-derived cell assays to dissect cellular interactions in human minor salivary glands across SjD severity and serological status.
Study design
Pranzatelli and colleagues analyzed minor salivary gland biopsies from patients with SjD and from non-SjD controls using a multimodal approach: single-cell RNA sequencing (scRNA-seq), spatial transcriptomics, and spatial immunophenotyping. They correlated cellular and spatial changes with clinical metrics including anti-SSA positivity and focus score (a histopathologic index of lymphocytic infiltration). To test mechanisms inferred from these datasets, the group established patient-derived primary epithelial cell cultures and performed autologous co-cultures with T cells isolated from the same individuals. Ex vivo stimulation and functional assays (including mitochondrial integrity, degranulation, and interferon pathway activation) were used to examine the effector functions of GZMK-expressing CD8+ T cells.
Primary endpoints were descriptive and mechanistic: identification of glandular cell populations altered in SjD, characterization of infiltrating immune cell states, spatial co-localization of immune and epithelial cell types, and functional validation of effector mechanisms in vitro.
Key findings
1. Discovery of acinar cell heterogeneity and selective loss of a seromucous acinar subtype
High-resolution scRNA-seq revealed previously unappreciated heterogeneity among acinar epithelial cells in human minor salivary glands. One defined cluster — characterized by PRR4 positivity, CST3 expression, and absence of WFDC2 (noted as PRR4⁺CST3⁺WFDC2⁻) — corresponded to a seromucous acinar phenotype. Spatial transcriptomics and immunophenotyping showed that this acinar subset is selectively depleted in SjD patients compared with non-SjD controls. The degree of depletion correlated with clinical severity measures, suggesting a link between loss of this acinar population and glandular dysfunction.
Clinical significance: Identifying discrete acinar subtypes that are selectively vulnerable provides a cellular target for understanding loss of secretory function and opens potential for cell-protective strategies.
2. GZMK⁺CD8⁺ T cells are enriched with disease severity and display a cytotoxic but sub-lytic program
The immune landscape in affected glands differed by clinical endotype. Patients who were anti-SSA (Ro) antibody–positive with high focus scores demonstrated T cells with increased transcriptional signatures of activation, enhanced antigen-presentation pathways, and features suggesting apoptosis resistance. Across samples, a distinct population of GZMK-expressing CD8+ T cells accumulated in proportion to disease severity.
Transcriptionally, these GZMK⁺CD8⁺ cells expressed cytotoxic machinery but did not fit the canonical fully lytic GZMB-dominant profile. Instead, they exhibited a program consistent with degranulation potential and proinflammatory mediator release without overt perforin-driven lytic signatures.
3. Spatial co-localization and immune-engaged epithelial states
Spatial analyses demonstrated that GZMK⁺CD8⁺ T cells preferentially localized adjacent to epithelial regions marked by interferon-stimulated gene (ISG) expression and other markers of immune engagement. Patients with lower overall immune infiltration displayed distinct epithelial organization, implying that epithelial-immune crosstalk varies across clinical presentations and might shape both histologic appearance and symptoms.
4. Functional validation: GZMK affects epithelial mitochondria and activates interferon signaling
In vitro assays provided mechanistic support for a sub-cytolytic effector role of GZMK. Recombinant or T cell–delivered GZMK triggered mitochondrial perturbations in primary patient-derived epithelial cells and induced type I interferon pathway activation. Autologous co-cultures of patient-derived T cells with epithelial cells recapitulated these effects and confirmed that GZMK delivery, not classical perforin-mediated lysis, best explained the observed epithelial transcriptional changes.
Taken together, these data support a model in which GZMK⁺CD8⁺ T cells mediate targeted epithelial injury that is non-lytic yet sufficient to impair mitochondrial function and stimulate innate antiviral-like responses, including type I interferon signaling — a pathway long implicated in SjD pathogenesis.
Expert commentary and mechanistic insights
The study integrates high-dimensional atlasing with functional validation, an approach that strengthens causal inference beyond correlative single-cell observations. The identification of a selectively lost PRR4⁺CST3⁺ seromucous acinar subset refines the target cell concept in SjD: disease-associated epithelial remodeling is not uniform but cell type–specific. This has implications for regenerative strategies and biomarker development.
GZMK has emerged in recent years as an inflammatory granzyme with distinct biology from granzyme B. Unlike GZMB-driven lysis that requires perforin, GZMK can act extracellularly or within target cells via non-classical entry routes and promote inflammatory signaling. The observation that GZMK perturbs mitochondrial integrity and activates interferon pathways provides a plausible mechanistic bridge between immune attack and the prominent interferon signature observed in many SjD patients.
These findings align with broader concepts in autoimmunity where chronic, sub-lytic immune interactions drive sustained innate immune activation and tissue dysfunction rather than acute cell death. They also explain why glandular biopsies may show extensive epithelial activation with variable cell loss and why therapies targeting adaptive immunity alone produce inconsistent results.
Limitations worth noting: the study is observational for tissue profiling and in vitro for mechanistic work, so in vivo causal proof remains to be established. The cell-culture system models key interactions but cannot fully reconstitute tissue architecture, stromal contributions, or systemic immune regulation. Sample sizes and cohort diversity may limit generalizability to all SjD subtypes; longitudinal data would strengthen claims about progression.
Clinical and translational implications
– Biomarkers and endotyping: Loss of the PRR4⁺CST3⁺ acinar population and enrichment of GZMK⁺CD8⁺ T cells correlate with serological and histologic severity; combining single-cell–derived markers with conventional metrics (anti-SSA status, focus score) could refine patient stratification.
– Therapeutic targets: The data nominate several intervention points: (1) neutralization or inhibition of GZMK activity; (2) approaches to preserve mitochondrial health in acinar cells; (3) modulation of type I interferon signaling (e.g., anti-IFNAR strategies); and (4) selective modulation of pathogenic CD8+ T cells while preserving antiviral immunity. Existing agents that target the IFN pathway or T-cell activation could be evaluated in biomarker-selected cohorts.
– Regenerative approaches: Defining vulnerable acinar subtypes informs regenerative therapy design. Cell therapies or agents that specifically support the PRR4⁺CST3⁺ seromucous lineage may have higher yield for restoring secretory function.
Conclusion
Pranzatelli et al. provide a compelling single-cell and spatially resolved map of immune–epithelial interactions in human minor salivary glands in Sjögren’s disease. The work identifies a selectively lost seromucous acinar population and highlights GZMK⁺CD8⁺ T cells as key effectors that impair mitochondrial integrity and induce interferon-driven epithelial dysfunction through a sub-cytolytic mechanism. These insights refine disease endotyping, clarify pathogenic mechanisms that link targeted epithelial injury to chronic innate immune activation, and point to novel therapeutic strategies that merit preclinical and clinical evaluation.
Funding and trial registration
Funding and detailed trial registration information are as reported in the original publication: Pranzatelli TJF et al., Ann Rheum Dis. 2025. Readers should consult the source article for full disclosure of funding sources and ethics approvals.
Selected references
– Pranzatelli TJF, Perez P, Ku A, et al. GZMK+CD8+ T cells target a specific acinar cell type in Sjögren’s disease. Ann Rheum Dis. 2025 Oct 28:S0003-4967(25)04313-4. doi:10.1016/j.ard.2025.08.014.
– Fox RI. Sjögren’s syndrome. Lancet. 2005;366(9482):321-331.
– Mavragani CP, Moutsopoulos HM. Sjögren’s syndrome. Annu Rev Pathol. 2014;9:273-285.