Highlight
- World’s first genetically engineered pig auxiliary liver xenotransplantation performed successfully in a living human for 171 days.
- The 10-gene edited porcine liver demonstrated functional metabolic activity and coagulation correction without hyperacute rejection.
- Xenotransplantation-associated thrombotic microangiopathy (xTMA) identified as a major postoperative complication, managed with eculizumab and plasma exchange.
- This pioneering case provides critical insights into immunological and coagulation challenges, paving the way for future clinical liver xenotransplantation.
Study Background
Organ transplantation remains the definitive treatment for end-stage liver disease and select hepatic malignancies; however, donor organ shortage severely limits timely access, often resulting in high mortality. While genetically engineered pig-to-human xenotransplantation has garnered attention primarily in cardiac and renal domains, porcine liver xenotransplantation has not been clinically realized until now. The liver’s complex immunological milieu and unique coagulation profile pose substantial barriers to xenogeneic transplantation, necessitating advanced genetic modifications and careful perioperative management. This report documents the world’s first clinical execution of auxiliary genetically modified pig liver transplantation in a living human, addressing the critical unmet need for bridge therapy in hepatocellular carcinoma patients unsuitable for resection or immediate allotransplantation.
Study Design
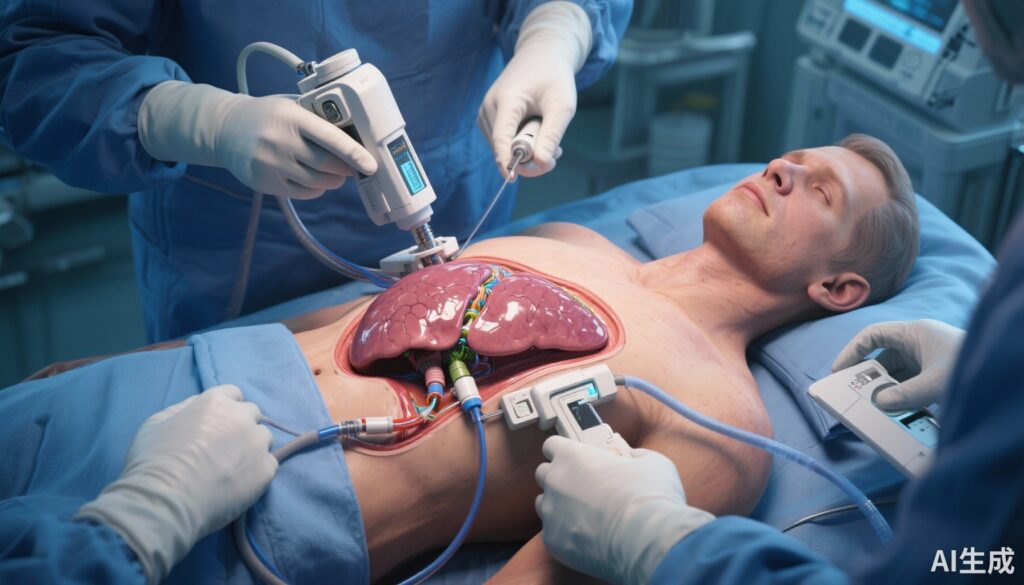
The study involves a single-patient case undergoing auxiliary liver transplantation using a genetically engineered pig liver harboring 10 targeted gene edits. These modifications included knockout of porcine xenoantigen genes responsible for hyperacute rejection and the knock-in of seven human transgenes conferring improved immunological and coagulation compatibility. The recipient was a patient with large hepatocellular carcinoma localized to the right hepatic lobe, initially deemed ineligible for curative resection and immediate human liver transplantation.
Postoperatively, the patient was closely monitored with serial assessments of liver function tests, metabolic markers, and coagulation parameters. The primary endpoint was the viability and function of the auxiliary xenograft without immunological rejection or life-threatening complications. Secondary endpoints included management of coagulation abnormalities and long-term survival.
Key Findings
The auxiliary porcine liver functioned effectively, evidenced by demonstrated metabolic activity, bile production, and partial correction of coagulation disturbances, stabilizing the recipient’s condition for the initial 31 days without signs of hyperacute or acute rejection, infection, or significant morbidity. Liver and renal function remained stable during this period, highlighting the graft’s physiological compatibility and immunological tolerance achieved by the extensive genetic engineering.
Early postoperative coagulopathy, indicated by elevated D-dimer and fibrin degradation products, was effectively managed with anticoagulant therapy, emphasizing the importance of proactive coagulation control given the liver’s critical role in hemostasis. However, thrombosis-related complications emerged by postoperative day 38, necessitating removal of the auxiliary liver due to xenotransplantation-associated thrombotic microangiopathy (xTMA), characterized by endothelial injury, microvascular thrombosis, and hemolytic anemia.
Subsequent treatment with complement inhibition via eculizumab and plasma exchange successfully resolved the xTMA, underscoring the potential for immunomodulatory therapeutic strategies to manage xenotransplant complications. Despite the initial success, recurrent upper gastrointestinal hemorrhage occurred, ultimately culminating in the patient’s death on postoperative day 171. The cause highlights ongoing challenges with vascular integrity and bleeding risk in the context of xenotransplantation.
Expert Commentary
The pioneering use of a 10-gene edited pig liver as an auxiliary graft in a living human patient reveals both promising opportunities and formidable challenges in the field of clinical liver xenotransplantation. The genetic modifications employed—targeting xenoantigens and incorporating human genes relevant to immune modulation and coagulation pathways—represent a sophisticated synthetic biology approach essential for overcoming xenograft rejection and dysfunction.
The observation of xTMA in a living recipient is particularly noteworthy as it delineates a previously underrecognized complication with significant clinical implications. The successful reversal of this condition with complement blockade and plasma exchange provides a critical mechanistic insight and therapeutic avenue for future cases.
Nevertheless, the fatal outcome due to repeated gastrointestinal bleeding underscores the need for enhanced strategies to manage post-xenotransplant hemostatic perturbations and vascular fragility. Limitations of this single-case study include the lack of long-term graft function and survival data from a broader cohort, warranting cautious interpretation and reinforcing the imperative for controlled trials.
Conclusion
This landmark clinical case establishes the feasibility of genetically engineered pig-to-human auxiliary liver xenotransplantation as a bridge therapy in liver malignancy patients. The findings demonstrate the potential for metabolic function and coagulation support from xenografts engineered for immune compatibility. However, xenotransplantation-associated thrombotic microangiopathy remains a critical obstacle to sustained success, necessitating further research to optimize immunosuppression, graft engineering, and perioperative management.
Future directions should focus on expanding gene editing platforms to further mitigate immune and coagulation-related complications, and rigorous clinical trials to evaluate safety and efficacy. This pioneering effort marks a significant milestone in transplant medicine and synthetic biology, offering hope for addressing the dire organ shortage and improving outcomes in liver disease and cancer.
Funding and Clinical Trials
Details on funding sources and clinicaltrial.gov registration were not provided in the reference article.
References
Zhang W, Xu Q, Xu K, Jiang R, Wang S, Zheng M, Liu N, Jiao D, Wang Z, Ge J, Lu X, Li G, Huang F, Liu L, Yin Y, Liu Y, Guo J, Liu K, Wei HJ, Sun B. Genetically engineered pig-to-human liver xenotransplantation. J Hepatol. 2025 Dec 1:S0168-8278(25)02497-3. doi: 10.1016/j.jhep.2025.08.044. Epub ahead of print. PMID: 41076089.