Highlight
- Hyperinsulinemia inversely correlates with fractional excretion of urate (FEUA), implicating URAT1-mediated urate reabsorption in hyperuricemia.
- Phosphorylation of URAT1 at Thr408 by AKT and SGK1 kinases, induced by hyperinsulinemia and high salt intake, respectively, increases URAT1 activity and serum urate levels.
- Genetic variants of SLC22A12 (notably rs147647315 and rs475688) modulate the impact of hyperinsulinemia on serum urate, highlighting gene-environment interactions.
- These findings support personalized approaches to hyperuricemia treatment considering metabolic status and genetic background.
Study Background and Disease Burden
Hyperuricemia, characterized by elevated serum urate levels, is strongly heritable and a central risk factor for gout, a common and painful inflammatory arthritis. It frequently coexists with insulin resistance and hyperinsulinemia, features of metabolic syndrome, but the precise molecular mechanisms linking hyperinsulinemia to altered urate metabolism remain unclear. Understanding how genetic factors and environmental influences such as salt intake modify urate homeostasis is critical to developing personalized and effective therapeutic strategies for hyperuricemia and related complications.
Study Design
This study incorporated a multi-tiered approach. Clinically, among 162 outpatient participants, researchers evaluated the association between an index of hyperinsulinemia (indicative of insulin levels and resistance) and the fractional excretion of urate (FEUA), a measure of renal urate clearance. To decipher molecular mechanisms, single-cell transcriptomic analyses and kinase activity screens were conducted, complemented by cell culture experiments assessing URAT1 regulation.
Furthermore, a large-scale genetic epidemiology analysis was performed in 377,358 participants from the UK Biobank (UKBB). The study examined serum urate, markers of hyperinsulinemia (TyG index), and self-reported salt intake. Single nucleotide variants (SNVs) in SLC22A12, encoding the urate transporter URAT1, were evaluated for gene-environment interactions influencing serum urate levels.
Key Findings
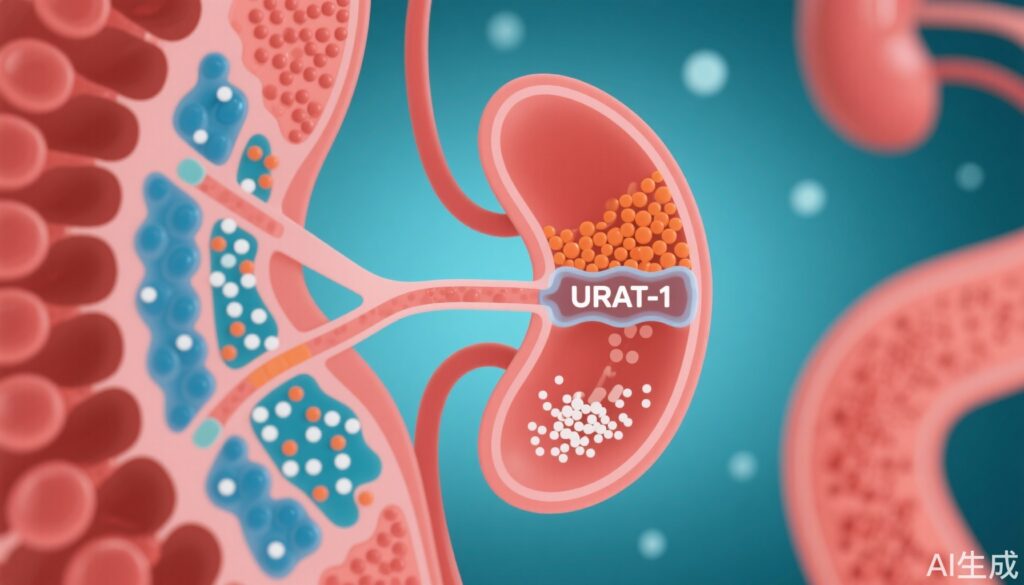
Clinically, the hyperinsulinemia index was significantly inversely associated with FEUA, independent of confounders, indicating reduced renal urate clearance with increased insulin levels.
Mechanistic insights revealed that URAT1’s abundance on the cell surface and its urate transport activity were regulated by phosphorylation at threonine 408, catalyzed by the serine/threonine kinases AKT (activated by hyperinsulinemia) and SGK1 (induced by high salt intake). Arg405 residue was critical for kinase-mediated phosphorylation, underscoring the specific molecular target. This phosphorylation enhanced URAT1’s function, promoting urate reabsorption.
The epidemiological analysis in UKBB confirmed independent associations of hyperinsulinemia and high salt intake with elevated serum urate. Both environmental factors convergently activate pathways that increase URAT1-mediated urate retention.
Genetic analysis identified that carriers of the SLC22A12 variant rs147647315 exhibited significantly lower serum urate levels, with this effect stronger than that of the common rs475688 SNP. Importantly, interaction analyses showed a trend towards a significant negative gene-environment interaction between the TyG index and rs147647315 (β = -7.50, P=0.096), suggesting that this variant attenuates the hyperinsulinemia-driven serum urate increase. Conversely, rs475688 functioned as an expression quantitative trait locus (eQTL) synergistically enhancing the positive association of serum urate with hyperinsulinemia.
The study also highlights the importance of other urate transporters, such as GLUT9 encoded by SLC2A9, whose mutations cause renal hypouricemia type 2, reinforcing the complex genetic landscape of urate metabolism.
Expert Commentary
This comprehensive research elucidates a biochemical and genetic nexus whereby hyperinsulinemia and dietary salt synergistically regulate URAT1 via phosphorylation, modulating renal urate handling. The identification of key phosphorylation sites and relevant kinases (AKT and SGK1) offers actionable molecular targets.
Moreover, integrating genetic data reveals that common and rare variants in SLC22A12 can modulate individual susceptibility to hyperuricemia in the context of metabolic and environmental exposures. These findings align with emerging paradigms that gene-environment interactions critically influence complex metabolic traits.
Clinicians should consider the metabolic profile, dietary habits, and genetic background when managing hyperuricemia, especially in patients with insulin resistance or metabolic syndrome. However, the study’s observational nature and genetic association trends (some marginally significant) require cautious interpretation, and future interventional studies are warranted.
Conclusion
The study compellingly demonstrates that URAT1, encoded by SLC22A12, mediates the association between hyperinsulinemia and hyperuricemia through phosphorylation-dependent regulation influenced by both metabolic and environmental factors. Genetic variants further modulate this interaction, providing a molecular basis for personalized hyperuricemia management.
These insights pave the way for targeted therapeutic strategies that consider patient-specific genetic makeup, insulin status, and lifestyle factors such as salt intake, potentially improving clinical outcomes for gout and related metabolic disorders.
References
Fujii W, Yamazaki O, Hirohama D, et al. Gene-environment interaction modifies the association between hyperinsulinemia and serum urate levels through SLC22A12. J Clin Invest. 2025 Mar 18;135(10):e186633. doi:10.1172/JCI186633 IF: 13.6 Q1 . PMID: 40100301 IF: 13.6 Q1 ; PMCID: PMC12077893 IF: 13.6 Q1 .