Highlight
– Roux-en-Y gastric bypass (RYGB) achieves greater and sustained reductions in weight and HbA1c than sleeve gastrectomy (SG) in patients with type 2 diabetes mellitus (T2DM).
– RYGB is associated with significant long-term reductions in all-cause mortality and obesity-related comorbidities compared to non-surgical controls.
– RYGB carries elevated risks of malabsorption, micronutrient deficiencies, alcohol use disorder, psychiatric disorders, and surgical complications.
– SG shows comparable weight loss to RYGB but lacks significant effects on obesity-related comorbidities and surgical complication risks.
Study Background
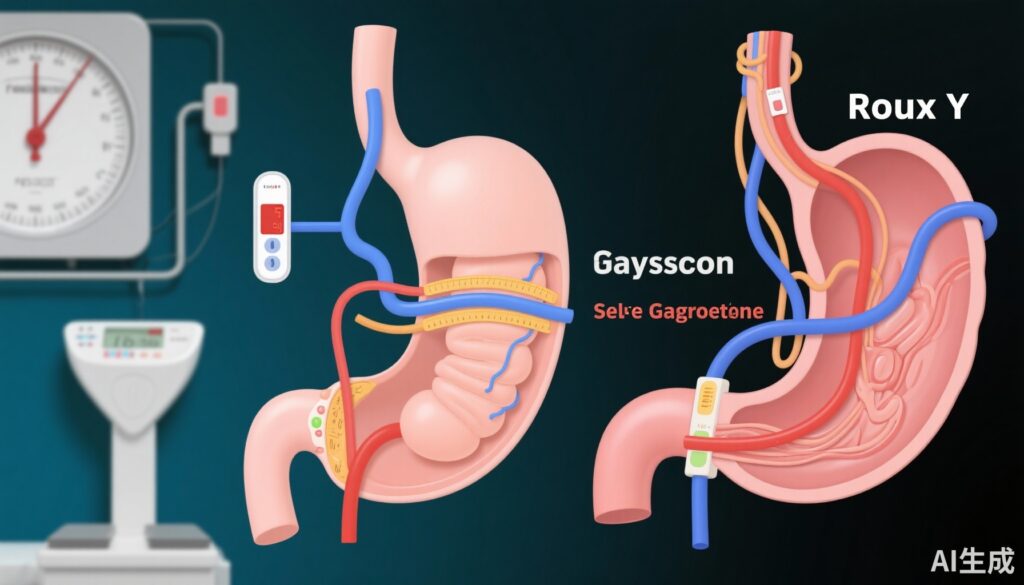
Type 2 diabetes mellitus (T2DM) is a prevalent chronic disorder closely linked with obesity, imposing a substantial burden through associated morbidity and mortality worldwide. Bariatric surgery, notably Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG), has emerged as an effective treatment modality for obesity and T2DM, promoting weight reduction and glycemic control. However, long-term comparative data evaluating both efficacy and safety of RYGB and SG, especially in real-world settings, remain limited, complicating clinical decision-making. Understanding long-term impacts on diabetes remission, mortality, and surgery-related complications is critical to optimize patient selection and postoperative management.
Study Design
This retrospective, matched cohort study utilized comprehensive nationwide Swedish registries: the Swedish National Diabetes Register (NDR) and the Swedish Obesity Surgery Registry (SOReg). Eligible adults with T2DM undergoing primary bariatric surgery from 2007 to 2020 were identified (RYGB n=7294, SG n=1105). These surgical cohorts were matched 1:1 with non-surgical controls from the NDR on age, sex, body mass index (BMI), and diabetes duration, totaling 8399 controls. Outcomes examined over up to 14 years included total weight loss percentage (%TWL), glycemic control measured via HbA1c, all-cause mortality, obesity-related morbidity, micronutrient deficiencies, alcohol use disorder, psychiatric disorders, and surgical complications. Adjusted Cox regression models accounting for diabetes duration and other covariates estimated hazard ratios (HRs) with 95% confidence intervals (CIs).
Key Findings
Weight Loss and Glycemic Control:
Both RYGB and SG groups demonstrated markedly greater %TWL compared to matched controls at two years post-procedure (RYGB: 23.2% vs. 3.6%; SG: 17.1% vs. 3.1%). Correspondingly, mean HbA1c levels showed significant reductions after surgery (RYGB: 46 mmol/mol vs. 58; SG: 46 vs. 55), indicating improved glycemic control with sizable effect sizes (standardized mean differences >0.1). Notably, RYGB induced more robust and sustained glycemic improvements relative to SG.
All-Cause Mortality and Comorbidities:
RYGB was associated with a substantial 38% reduction in all-cause mortality compared with non-surgical controls (adjusted HR 0.62, 95% CI 0.51–0.71). Furthermore, RYGB recipients experienced up to 45% lower incidence of obesity-related comorbidities, demonstrating durable health benefits. In contrast, SG did not significantly reduce mortality or obesity-related disease risks versus controls despite effective weight loss.
Risks and Complications:
The advantages of RYGB were tempered by increased risks of adverse outcomes. The procedure doubled the risk of malabsorption and micronutrient deficiencies (adjusted HR 2.00 [1.76–2.28]) and nearly tripled the incidence of alcohol use disorder (adjusted HR 2.82 [2.37–3.36]) relative to controls. Psychiatric disorders such as depression were also elevated after RYGB (adjusted HR 1.28 [1.14–1.43]). Surgical complications, notably bowel obstruction, occurred at a nearly 4-fold higher rate post-RYGB (adjusted HR 3.96 [3.15–4.98]). Conversely, SG patients did not exhibit significant increases in these complications.
Expert Commentary
This robust, population-based study leverages matched cohorts and extended follow-up to yield compelling evidence on the comparative long-term effectiveness and safety of RYGB versus SG in T2DM individuals. The findings corroborate prior clinical data that RYGB offers superior metabolic outcomes and survival benefits compared to SG or nonsurgical management. Elevated complication risks following RYGB highlight the importance of comprehensive postoperative surveillance and individualized risk-benefit assessment. The absence of significant obesity-related morbidity reductions after SG, despite good weight loss, suggests a differential metabolic impact that warrants further mechanistic exploration. Limitations include the observational design with residual confounding potential and unequal group sizes. Nevertheless, these real-world data provide crucial insights to guide surgical choice and optimize outcomes in T2DM patients.
Conclusion
In conclusion, RYGB confers profound and durable benefits in weight reduction, glycemic control, and survival among people with T2DM, albeit accompanied by increased nutritional and psychiatric risks. SG achieves comparable weight loss but does not significantly influence long-term obesity-related comorbidities or mortality. These findings emphasize the need for tailored surgical decision-making that balances efficacy with safety, informed by individual patient risk profiles and preferences. Future research should focus on elucidating the biological mechanisms underlying divergent outcomes and developing strategies to mitigate post-RYGB complications.
Funding and Trial Registration
This study was funded by a grant from the Swedish state under the agreement with county councils. No clinical trial registration was reported due to its retrospective design.