Highlights
- Long-term exposure to fine particulate matter (PM2.5) was associated with a 3.35-fold increased risk for incident systemic lupus erythematosus (SLE) in Taiwanese adults.
- Risk increased linearly across all age and sex groups, with women and former smokers showing even higher susceptibility.
- Findings reinforce the public health imperative for policies aimed at reducing PM2.5 exposure to lower SLE incidence.
Study Background and Disease Burden
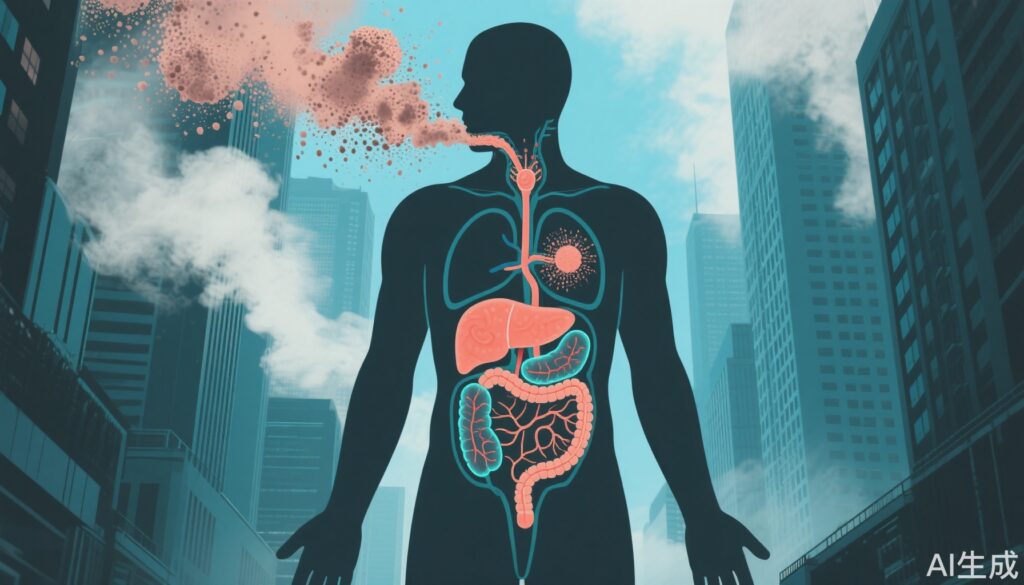
Systemic lupus erythematosus (SLE) is a chronic, multisystem autoimmune disorder with significant morbidity and mortality. While genetic factors are well-established contributors, environmental determinants—including air pollution—are increasingly implicated in autoimmune disease pathogenesis. Fine particulate matter (PM2.5), defined as airborne particles with a diameter less than 2.5 micrometers, is a recognized public health hazard linked to cardiovascular, respiratory, and now autoimmune diseases. Given the rising prevalence of SLE and the ubiquity of air pollution in East Asia, clarifying the link between PM2.5 exposure and incident SLE is of significant clinical, public health, and policy relevance.
Study Design
Researchers conducted a prospective, longitudinal cohort study in Taiwan, leveraging national registry data and environmental monitoring systems. The cohort included 268,254 adults (mean age: 39.3 years; 51% women) recruited between 2005 and 2017. Participants were followed for an average of 9.8 years. Incident SLE was defined using a validated national registry, ensuring diagnostic accuracy. Annual average PM2.5 concentrations were estimated at each participant’s residential address using Taiwan’s air quality-monitoring database, permitting individualized exposure assessment. Covariates included age, sex, and smoking status.
Key Findings
Over the follow-up period, 151 participants (0.1%) developed new-onset SLE, corresponding to an incidence rate of 5.75 cases per 100,000 person-years. The primary finding was a robust association between PM2.5 exposure and risk of SLE: each 5-µg/m3 increment in mean annual PM2.5 was linked to a 3.35-fold increased risk of incident SLE (adjusted hazard ratio [aHR], 3.35; 95% CI, 2.94-3.82). This association demonstrated a clear linear dose-response relationship across all age and sex subgroups.
Notably, female sex emerged as a powerful independent risk factor for SLE (aHR, 10.00; 95% CI, 5.56-16.67), consistent with established epidemiology. Former smokers also had an elevated risk (aHR, 2.59; 95% CI, 1.23-5.48). The findings were robust after adjusting for confounders.
No significant interactions between PM2.5 exposure and other demographic factors were detected, suggesting broad generalizability within the Taiwanese adult population.
Expert Commentary
The study by Lai and colleagues provides compelling evidence for PM2.5 as a modifiable environmental risk factor for SLE. The use of a large, well-characterized cohort with long-term follow-up and individualized exposure assessment strengthens causal inference. The clear dose-response relationship across demographic strata supports biological plausibility, potentially mediated by PM2.5-induced systemic inflammation, oxidative stress, and immune dysregulation—mechanisms previously linked to autoimmune disease initiation and exacerbation.
However, several limitations should be noted. The observational design precludes definitive causal conclusions, and residual confounding (such as unmeasured socioeconomic or occupational exposures) may persist. The study is also geographically limited to Taiwan, and findings may not fully extrapolate to populations with different genetic backgrounds or air pollution profiles. Finally, the relatively low absolute incidence of SLE, despite high relative risks, should be contextualized in public health planning.
Conclusion
This Taiwanese cohort study robustly identifies long-term exposure to fine particulate matter (PM2.5) as a significant risk factor for developing systemic lupus erythematosus. Risk is particularly pronounced among women and former smokers. These findings underscore the urgent need for effective air quality policies to mitigate SLE incidence and highlight the broader intersection between environmental health and autoimmune disease. Further research should explore underlying mechanisms and validate these associations in diverse populations.
References
1. Lai YJ, Chen LJ, Lin YK, Wang SF, Chen MJ, Lee JJ, Chen CC, Chen YT, Chung PY, Hsu LF, Lai KZ, Ahmadi MN, Inan-Eroglu E, Koemel NA, Yen YF, Ku PW. Higher PM2.5 exposure increases the risk of incident systemic lupus erythematosus: a prospective cohort study in Taiwan. Lupus Sci Med. 2025 Jul 20;12(2):e001385. doi: 10.1136/lupus-2024-001385 IF: 3.5 Q2 . PMID: 40685228 IF: 3.5 Q2 ; PMCID: PMC12278130 IF: 3.5 Q2 .
2. Costenbader KH, et al. Environmental exposures and risk of systemic lupus erythematosus. Curr Opin Rheumatol. 2020;32(5):482-489.3. Yang BY, et al. Long-term exposure to ambient air pollution and risk of autoimmune diseases: a nationwide cohort study in China. Environ Pollut. 2022;309:119748.