Background
Cancer-associated venous thromboembolism (VTE), comprising pulmonary embolism (PE) and deep vein thrombosis (DVT), represents a significant contributor to morbidity and mortality among patients with active malignancy. As cancer incidence rises alongside improved cancer survival, managing thrombotic complications has become increasingly critical. While anticoagulants remain the mainstay for VTE treatment, adjuvant therapies aiming to reduce VTE recurrence and mortality are actively investigated. Aspirin, renowned for its antiplatelet effects, is widely used for primary thromboprophylaxis in cancer subpopulations and has shown anticancer properties in various studies. However, its efficacy and safety when used adjunctively with anticoagulants in treating established cancer-associated VTE remain unclear. This retrospective multicenter study was undertaken to elucidate the role of low-dose aspirin as an adjuvant therapy in this high-risk context.
Study Design and Methods
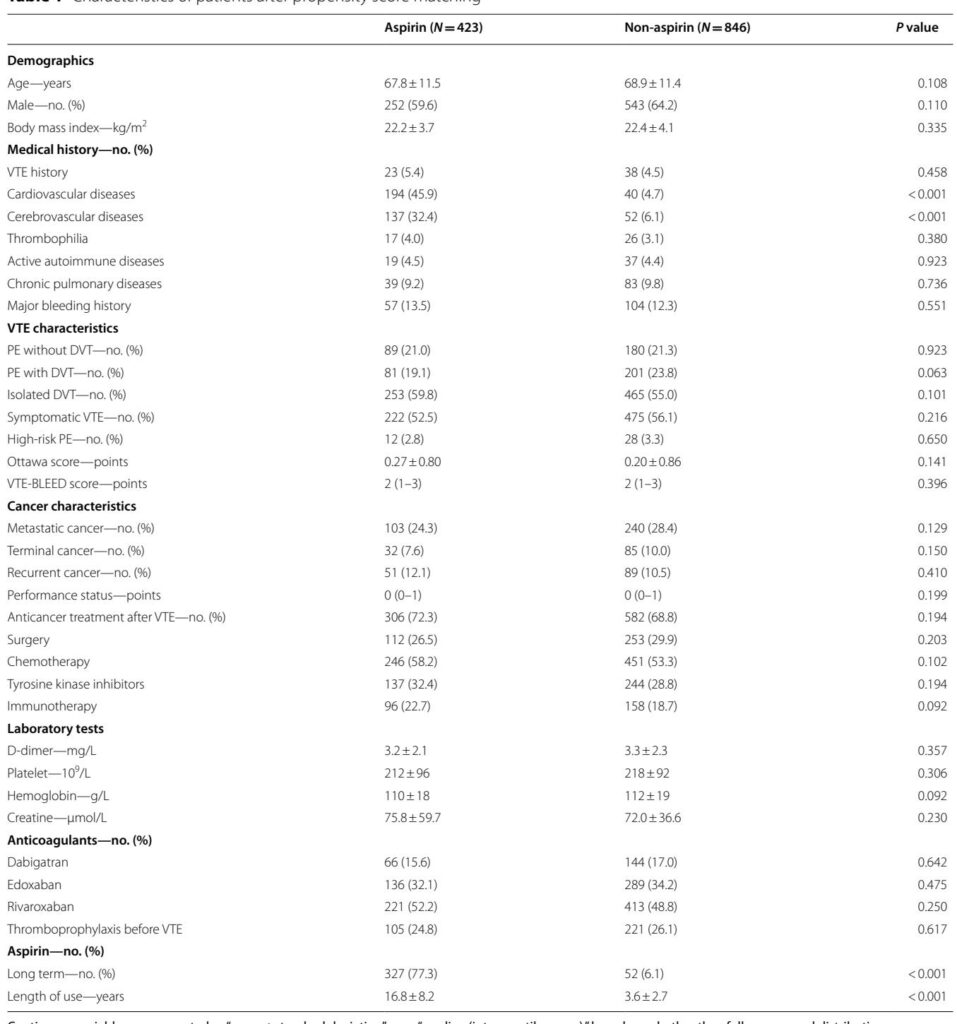
The study encompassed 2358 patients with active cancer and objectively confirmed acute VTE from multiple centers between May 2017 and May 2024. Patients were divided into two cohorts: those receiving conventional direct oral anticoagulants (DOACs) alone and those receiving DOACs plus daily low-dose aspirin (100 mg). Key inclusion criteria included age ≥18, histologically confirmed active cancer, standard DOAC therapy for at least 6 months post-VTE diagnosis, and appropriate anticancer treatment. Exclusion criteria eliminated patients with chronic thromboembolic disease or non-low-dose aspirin/alternative antiplatelet therapies.
To minimize confounding, propensity score matching (1:2 ratio) was utilized to balance demographics, comorbidities, cancer types, VTE-related risk factors, anticoagulant regimens, and bleeding risk scores. The primary endpoint was VTE recurrence at 6 months, defined by imaging demonstration of new or progressive thrombosis. Secondary endpoints included PE-related mortality, all-cause mortality, and major bleeding as per ISTH criteria. Net clinical benefit (NCB) was a composite endpoint of absence of VTE recurrence, major bleeding, and death.
Key Findings
Following propensity matching, 1269 patients (aspirin group, n=423; non-aspirin group, n=846) were analyzed. Aspirin adjunctive therapy was associated with a significantly lower 6-month VTE recurrence rate (3.1% vs 6.5%; HR 0.55; 95% CI 0.30–0.99; P=0.011) and reduced PE-related mortality (2.8% vs 5.4%; HR 0.54; 95% CI 0.28–0.91; P=0.037). However, no significant difference was observed in all-cause mortality (25.5% vs 27.0%; HR 0.98; 95% CI 0.78–1.24; P=0.887).
Importantly, the aspirin group experienced a significantly higher rate of major bleeding events (12.3% vs 5.4%; HR 2.45; 95% CI 1.65–3.64; P<0.001). Consequently, there was no observed improvement in net clinical benefit between groups (64.8% vs 65.5%; HR 0.98; 95% CI 0.80–1.19; P=0.812).
Subgroup analysis focusing on patients with PE failed to demonstrate statistically significant differences in VTE recurrence or PE-related mortality with adjunctive aspirin, possibly due to residual confounding despite propensity matching.
Expert Commentary
This study is the first large-scale observational analysis addressing aspirin’s adjuvant role beyond primary prophylaxis in cancer-associated VTE. The demonstrated reduction in VTE recurrence and PE-related mortality suggests a potential synergistic effect when aspirin is combined with anticoagulants, likely via its platelet inhibition augmenting standard anticoagulant pathways.
Nonetheless, the marked increase in major bleeding underscores the delicate hemostatic balance altered by dual antithrombotic therapy, especially in a cancer cohort inherently predisposed to bleeding complications. The absence of benefit in overall survival and net clinical benefit challenges the routine adoption of aspirin adjunctive therapy without individualized risk assessment.
Mechanistically, aspirin’s anticancer effects reported in long-term population studies may not manifest within the short 6-month window used here, explaining the lack of impact on all-cause mortality. Moreover, the predominance of long-term aspirin use in the aspirin group prior to VTE diagnosis complicates attribution of observed benefits to post-VTE aspirin initiation.
Limitations include retrospective design, potential residual confounding (notably comorbid cardiovascular and cerebrovascular disease prevalence), and lack of standardized follow-up protocols. The high utilization of DOACs over LMWH or VKAs restricts extrapolation to other anticoagulant therapies. Future randomized controlled trials (RCTs) are warranted to validate these findings and define optimal patient selection.
Conclusions
In patients with cancer-associated VTE, adjunctive low-dose aspirin with conventional anticoagulants is associated with a reduction in VTE recurrence and PE-related mortality at 6 months but comes at a significantly increased risk of major bleeding. No improvement in all-cause mortality or net clinical benefit was observed. Clinicians should carefully individualize the use of aspirin as adjunct therapy, weighing thrombotic risk reduction against bleeding hazards. Prospective RCTs are needed to establish definitive clinical guidelines.
References
1. Streif MB, Holmstrom B, Angelini D, et al. Cancer-associated venous thromboembolic disease, version 2.2021, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2021;19(10):1181–1201.
2. Farge D, Frere C, Connors JM, et al. 2022 international clinical practice guidelines for the treatment and prophylaxis of venous thromboembolism in patients with cancer, including patients with COVID-19. Lancet Oncol. 2022;23(7):e334–e347.
3. Brighton TA, Eikelboom JW, Mann K, et al. Low-dose aspirin for preventing recurrent venous thromboembolism. N Engl J Med. 2012;367(21):1979–1987.
4. Chen WY, Ballman KV, Partridge AH, et al. Aspirin vs placebo as adjuvant therapy for breast cancer: the Alliance A011502 randomized trial. JAMA. 2024;331(20):1714–1721.
5. Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020;41(4):543–603.