Highlight
• In a multicentre randomised superiority trial (NCT05548114), EUS‑guided gastroenterostomy (EUS‑GE) achieved substantially fewer poor clinical outcomes at discharge and during 6‑month follow‑up than surgical gastrojejunostomy (SGJ) for malignant gastric outlet obstruction (GOO).
• EUS‑GE patients resumed solid diet earlier (median 2 vs 5 days), had shorter hospital stays (median 3 vs 9 days), reported better physical and social functioning, and incurred lower treatment costs (US$33,934 vs US$51,437).
Background
Malignant gastric outlet obstruction is a frequent and disabling complication of advanced gastrointestinal malignancies—most commonly pancreatic, distal gastric, and duodenal cancers—and substantially impairs oral intake, nutritional status and quality of life. Palliation aims to relieve obstruction to permit oral nutrition, minimise procedure‑related morbidity, limit hospital time and avoid recurrent interventions.
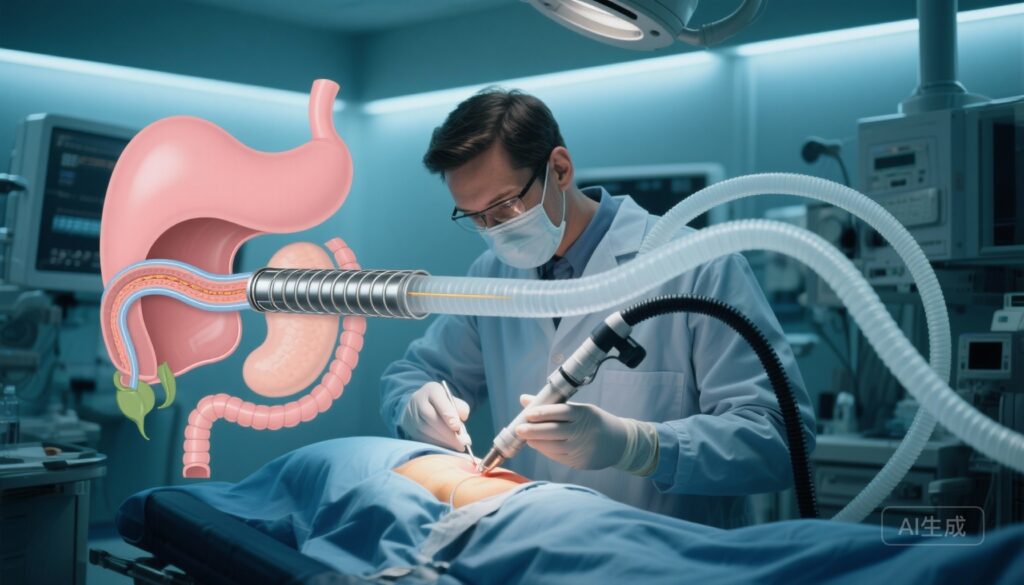
Historically, surgical gastrojejunostomy (SGJ) has been the definitive palliative bypass used to treat malignant GOO; it provides durable relief but is associated with operative stress, postoperative pain, prolonged recovery and health‑care resource use. Endoscopic alternatives include enteral stenting (self‑expanding metal stents across the obstructed duodenum) and, more recently, endoscopic ultrasound‑guided gastroenterostomy (EUS‑GE) using lumen‑apposing metal stents (LAMS) to create a direct anastomosis between the stomach and a jejunal loop. EUS‑GE is proposed to combine the durability of a bypass with the less invasive profile of endoscopic therapy, but high‑quality comparative data versus surgery have been limited.
Study design
The trial reported by Bang and colleagues (Gut, 2025) is a multicentre, randomised superiority study comparing EUS‑GE and SGJ in patients with malignant GOO. Patients were randomised to receive either EUS‑GE (n=38) or SGJ (n=36). The trial was registered at ClinicalTrials.gov (NCT05548114).
The primary endpoint was a composite, measured at hospital discharge and through 6 months (or until death): a Gastric Outlet Obstruction Scoring System (GOOSS) score of 0 or 1 at discharge (reflecting no oral intake or liquids only), the need for reinterventions or supplemental (parenteral or enteral) nutrition, or the occurrence of procedure‑related adverse events during follow‑up. Secondary endpoints included time to tolerating a solid diet, length of hospitalisation, health‑related quality of life (HRQoL), and total treatment costs.
Key findings
This trial found clinically and statistically meaningful advantages for EUS‑GE across the primary composite endpoint and most secondary outcomes.
Primary outcome
The primary composite endpoint occurred in 7.9% (3/38) of patients randomised to EUS‑GE versus 38.9% (14/36) of those randomised to SGJ. The absolute risk difference was −31.0% (95% CI −47.6% to −11.4%; p=0.002), favouring EUS‑GE. In other words, patients assigned to EUS‑GE were markedly less likely to have persistent poor oral intake at discharge, require repeat procedures or supplemental nutrition, or experience procedure‑related complications during follow‑up.
Time to oral intake and hospital stay
Patients undergoing EUS‑GE progressed to a solid diet substantially faster than those undergoing SGJ: median 2 days (interquartile range 2–3) versus 5 days (IQR 3.5–9). Hospital length of stay was shorter after EUS‑GE (median 3 days; IQR 3–6) than after SGJ (median 9 days; IQR 6–12.5). These are clinically meaningful reductions in recovery time and inpatient resource use.
Quality of life
Health‑related quality of life measures favoured EUS‑GE. The trial reported statistically significant improvements in physical functioning (p=0.0016) and social functioning (p=0.011) domains for patients treated with EUS‑GE versus SGJ, reflecting faster recovery and earlier resumption of normal activities and eating, which are particularly important in palliative care.
Costs
Treatment costs were substantially lower for EUS‑GE: mean US$33,934 versus US$51,437 for SGJ, a difference of −US$17,503 (95% CI −US$27,807 to −US$7,920). Reduced operating room time, shorter hospitalisation and fewer early complications likely contributed to this cost advantage.
Safety and reinterventions
The composite primary endpoint incorporated procedure‑related adverse events and need for reinterventions. The lower rate of primary endpoint events in the EUS‑GE arm implies fewer early complications and reinterventions overall. The report did not describe excess late stent‑related failures in the EUS‑GE group within the 6‑month window; longer follow‑up is necessary to fully compare durability. Mortality outcomes were reported as part of the 6‑month follow‑up but were not highlighted as different between groups in the summary data provided.
Expert commentary and interpretation
The results from this randomised, multicentre trial provide high‑quality comparative data that support EUS‑GE as an effective, less invasive alternative to surgical bypass for selected patients with malignant GOO. The magnitude of benefit across functional recovery, hospital stay, quality of life and costs is persuasive and clinically relevant, especially in the palliative setting where recovery time and preservation of quality of life are paramount.
Why might EUS‑GE perform better?
EUS‑GE creates a direct, fixed conduit between the stomach and a jejunal loop using a lumen‑apposing metal stent under endoscopic ultrasound guidance. Compared with SGJ, EUS‑GE avoids abdominal incision, general anaesthesia in some settings (though many procedures are performed under general anaesthesia), bowel mobilization, and the systemic inflammatory response consequent to surgery. These factors plausibly explain the faster return to oral intake, shorter inpatient recovery and better early quality‑of‑life scores in the EUS‑GE arm.
Clinical caveats and generalisability
Several important considerations temper the immediate generalisability of the findings. First, EUS‑GE requires specific expertise, advanced endoscopic skills and access to LAMS and dedicated equipment; outcomes depend strongly on operator experience and institutional volume. The trial was conducted at multiple centres likely proficient in advanced endoscopy, and the results may not extrapolate to centres without such expertise. Second, patient selection matters: anatomic factors (such as the degree of duodenal involvement, presence of extensive peritoneal carcinomatosis, or prior surgery) may preclude safe EUS‑GE in some patients and favour a surgical approach.
Third, the trial follow‑up was 6 months (or until death); while this is meaningful in many palliative contexts, longer observation is necessary to compare durability of symptom relief and late stent‑related complications (for example, stent migration, occlusion or buried stent issues) versus the long‑term patency of a surgical bypass. Fourth, surgical techniques vary (open vs laparoscopic approaches), and the trial summary did not detail whether SGJ procedures were predominantly laparoscopic or open; this can affect recovery times and costs.
Implications for practice
For patients with malignant gastric outlet obstruction who are candidates for endoscopic therapy and are treated in centres with experienced interventional endoscopists, EUS‑GE appears to offer a clinically meaningful and cost‑saving alternative to SGJ. EUS‑GE may be particularly attractive for patients with limited life expectancy where rapid improvement in oral intake, minimal hospital time and preservation of quality of life are priorities.
However, implementation should follow careful pathway planning: ensure appropriate patient selection, multidisciplinary discussion (surgical, oncology, nutrition and interventional endoscopy), formal operator training and access to rescue surgical services for complications. Centres adopting EUS‑GE should track outcomes including immediate technical success, time to oral intake, readmissions, reinterventions and longer‑term stent performance to confirm real‑world effectiveness and safety.
Limitations of the trial
Key limitations include the modest sample size (74 patients), which is adequate to detect the reported differences in the composite primary outcome but may be underpowered for less frequent adverse events or subgroup analyses. The composite primary endpoint includes diverse elements (GOOSS at discharge, need for reintervention or supplemental nutrition, and procedure‑related adverse events), and the relative contribution of each component to the observed difference was not dissected in the summary data. The trial’s 6‑month duration reflects a clinically relevant timeframe for many patients with advanced malignancy but does not address very long‑term durability. Finally, outcomes depend on operator skill; many centres will require training and experience to replicate these results.
Conclusion
This randomised multicentre trial demonstrates that EUS‑guided gastroenterostomy is superior to surgical gastrojejunostomy for palliation of malignant gastric outlet obstruction with respect to the composite of poor oral intake, need for reintervention or supplemental nutrition, and procedure‑related adverse events through 6 months. EUS‑GE also facilitated more rapid return to solid diet, shorter hospital stay, better short‑term quality of life and lower treatment costs. These findings support expanding the role of EUS‑GE in centres with appropriate expertise while highlighting the need for careful patient selection, training and longer‑term outcome data.
Funding and trial registration
Trial registration: NCT05548114. Funding details and full trial methodology and supplementary data are reported in the primary publication (see reference below).
References
Bang JY, Puri R, Lakhtakia S, Thakkar S, Waxman I, Siddiqui I, Arnold K, Chaudhary A, Mehta S, Singh A, Venkat Rao G, Basha J, Gupta R, Modak S, Singh S, Boone B, Dautel P, Dixon MEB, Kim HM, Sutton B, Arnoletti JP, Rösch T, Varadarajulu S. Endoscopic or surgical gastroenterostomy for malignant gastric outlet obstruction: a randomised trial. Gut. 2025 Sep 24:gutjnl-2025-336339. doi: 10.1136/gutjnl-2025-336339 IF: 25.8 Q1 . Epub ahead of print. PMID: 40998416 IF: 25.8 Q1 .