Study Background and Disease Burden
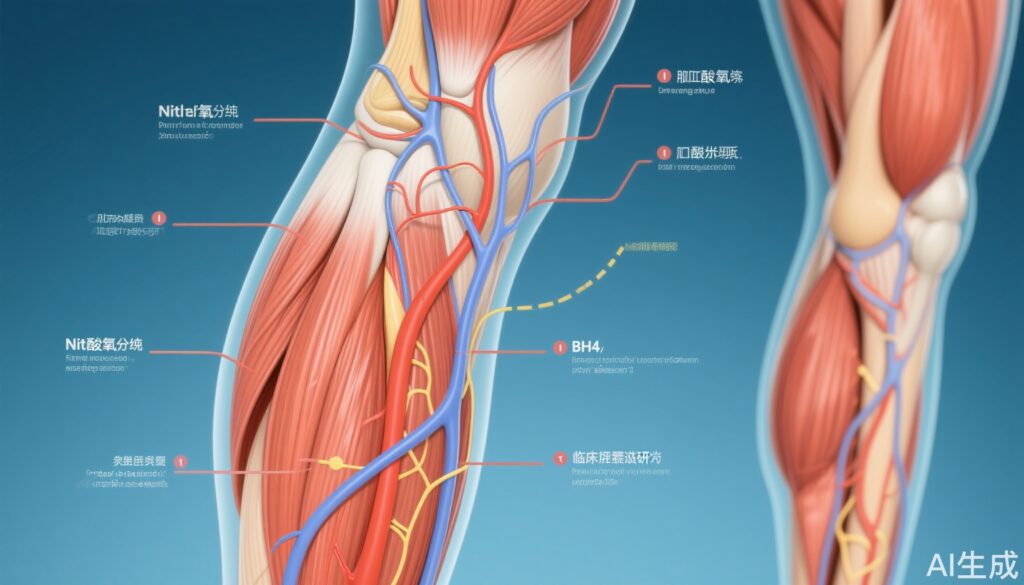
Peripheral microvascular dysfunction is a key pathophysiological feature observed in heart failure, encompassing both heart failure with reduced ejection fraction (HFrEF) and preserved ejection fraction (HFpEF). These dysfunctions contribute significantly to exercise intolerance and symptom burden in these populations. Impairments in nitric oxide (NO) signaling, partly due to tetrahydrobiopterin (BH4) deficiency and elevated oxidative stress, are implicated in compromising vascular endothelial function. BH4 is a critical cofactor for endothelial nitric oxide synthase (eNOS), facilitating NO production essential for microvascular dilation and perfusion. Concomitantly, oxidative stress promotes BH4 depletion and eNOS uncoupling, exacerbating endothelial dysfunction. Despite the recognition of these mechanisms, therapeutic strategies targeting NO bioavailability and oxidative stress remain underexplored in heart failure management. This study investigates the acute effects of enteral BH4 and antioxidant supplementation on locomotor muscle microvascular function in patients with HFrEF and HFpEF, addressing an unmet clinical need to improve peripheral vascular health and functional capacity.
Study Design
A randomized, double-blind, placebo-controlled crossover design was employed to evaluate the effects of acute enteral BH4 (10 mg/kg), an antioxidant cocktail (AOx), and their combined administration (BH4+AOx) on microvascular function. The study enrolled 33 patients, comprising 14 with HFrEF (mean age 64±10 years) and 19 with HFpEF (mean age 74±9 years). Microvascular function was assessed using passive limb movement (PLM), a non-invasive technique to gauge endothelial-dependent vasodilation in locomotor muscles by measuring changes in leg blood flow and hyperemic responses. Concurrently, circulating biomarkers of inflammation (C-reactive protein) and oxidative damage were quantified to explore potential systemic effects of interventions. Outcomes were compared to placebo control, with appropriate statistical analyses to discern treatment effects within each heart failure subgroup.
Key Findings
The principal outcome assessed was peak leg blood flow change during PLM. Compared with placebo, administration of AOx did not yield a significant difference in peak blood flow in either HFrEF (P=0.60) or HFpEF (P=0.61) patients. In contrast, BH4 alone significantly improved peak leg blood flow (P=0.033), with mean values increasing from 234±31 mL/min (placebo) to 357±45 mL/min (BH4) in HFrEF patients, and from 269±33 mL/min to 367±47 mL/min in HFpEF. Combined BH4+AOx treatment similarly enhanced peak blood flow compared to placebo (P=0.019) with comparable magnitude.
Assessment of the total hyperemic response (area under the curve of leg blood flow during PLM) revealed no statistical change with any treatment in the HFrEF cohort (P=0.29). However, HFpEF patients had a significant increase following BH4 (P=0.016) and BH4+AOx (P=0.040) relative to placebo, indicating improved sustained microvascular dilation.
Inflammatory biomarker analysis showed that C-reactive protein levels decreased significantly post-BH4 and BH4+AOx administration in HFpEF subjects (P=0.007), from 4268±547 ng/mL at baseline to approximately 2700 ng/mL post-treatment. No similar reduction was observed in HFrEF patients (P=0.39). These findings suggest anti-inflammatory effects of BH4 particularly in HFpEF.
Overall, acute antioxidant therapy alone did not enhance microvascular function or inflammation markers, nor did it augment the effects of BH4 when coadministered. This underscores the selective benefit of restoring BH4-dependent NO signaling rather than simply quenching oxidative stress in this setting.
Expert Commentary
This study provides compelling evidence for the role of the nitric oxide pathway, specifically through BH4 supplementation, in ameliorating locomotor muscle microvascular dysfunction common in heart failure phenotypes. The lack of impact from antioxidant therapy alone aligns with growing recognition that oxidative stress is a complex and not easily reversible contributor to endothelial dysfunction. The modest improvements in peak blood flow and inflammatory markers in HFpEF subjects may reflect underlying pathophysiological differences between HFpEF and HFrEF, particularly in vascular compliance and systemic inflammation.
Limitations include the relatively small sample size and the acute nature of the intervention, which may not reflect long-term therapeutic potential or translate directly into functional capacity enhancements. Additionally, while passive limb movement is a validated surrogate for endothelial function, direct measurement of exercise capacity was not performed.
Further research should explore chronic BH4 supplementation, dose optimization, and combined strategies targeting complementary mechanisms to improve vascular and clinical outcomes comprehensively.
Conclusion
In patients with heart failure, acute administration of tetrahydrobiopterin significantly improves key aspects of locomotor muscle microvascular function in both HFrEF and HFpEF, supporting the modulation of the nitric oxide pathway as a therapeutic avenue. By contrast, acute antioxidant administration alone or alongside BH4 does not confer vascular benefits, highlighting the specificity of BH4’s role in eNOS function. This insight advances our understanding of microvascular therapeutics in heart failure and indicates potential for BH4-focused interventions to alleviate peripheral vascular impairments and improve patient symptoms.