Highlight
- EUS-guided gastroenterostomy (EUS-GE) markedly reduces the need for reintervention at 6 months compared to uncovered duodenal metal stenting in malignant gastric outlet obstruction.
- Patients undergoing EUS-GE reported significantly better 1-month gastric outlet obstruction scores, reflecting improved oral intake capacity.
- No significant differences were noted in technical and clinical success rates, short-term mortality, or overall quality of life between the two interventions.
- Adverse event rates were comparable, with procedure-related pneumonia being infrequent in both groups.
Study Background and Disease Burden
Malignant gastric outlet obstruction (GOO) is a debilitating condition frequently encountered in patients with unresectable gastroduodenal or pancreatobiliary cancers. This obstruction significantly impairs oral nutrition and quality of life. Conventional palliative management typically involves placement of uncovered duodenal metal stents to restore luminal patency. However, stent dysfunction—due to tumor ingrowth, overgrowth, or mechanical issues—often necessitates reintervention, imposing additional morbidity on patients with limited survival.
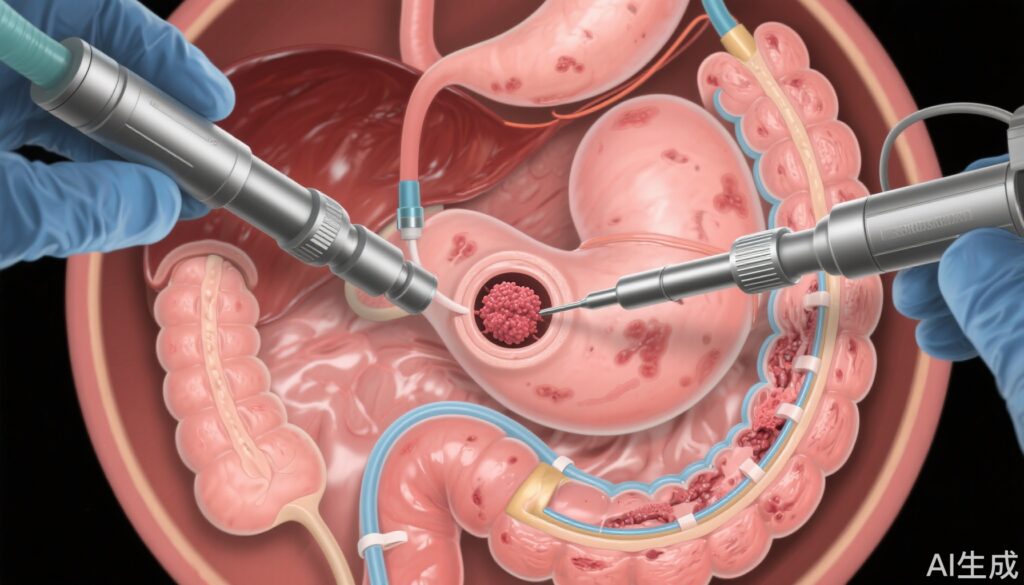
Endoscopic ultrasonography-guided gastroenterostomy (EUS-GE) is an innovative, minimally invasive technique creating a bypass between the stomach and a more distal jejunal segment, circumventing the obstructed region. The potential for improved long-term patency and decreased need for reintervention renders EUS-GE an attractive alternative to duodenal stenting, but robust comparative data have been lacking prior to the present trial.
Study Design
The DRA-GOO trial was an international, multicentre, prospective randomised controlled study conducted at seven tertiary centres across Hong Kong, Belgium, Brazil, India, Italy, and Spain. From December 2020 to February 2022, consecutive adult patients (≥18 years) with malignant GOO due to unresectable primary gastroduodenal or pancreatobiliary malignancies were enrolled. Eligible patients demonstrated a gastric outlet obstruction score (GOOS) of 0, indicating complete inability to intake food or liquids orally, and an Eastern Cooperative Oncology Group (ECOG) performance status ≤3.
Participants were randomly allocated 1:1 to receive either EUS-GE performed with a double balloon occluder device or conventional uncovered duodenal metal stenting. The primary endpoint was the rate of reintervention within 6 months, defined as additional endoscopic interventions necessitated by stent dysfunction, including restenosis from tumor ingrowth or overgrowth, stent migration, or fracture. Secondary outcomes included technical success (i.e., successful stent deployment), clinical success (≥1 point improvement in GOOS within 3 days), adverse events within 30 days, mortality within 30 days, stent patency duration, GOOS at 1 month, and patient-reported quality-of-life metrics.
Key Findings
Ninety-seven patients (48 EUS-GE, 49 duodenal stenting) were analysed following enrolment of 185 screened subjects. The mean age was 69.5 (SD 12.6) for the EUS-GE group and 64.8 (13.0) for the stenting group.
– Primary outcome: Reintervention was required in 2 patients (4%) in the EUS-GE group compared to 14 patients (29%) in the duodenal stenting group (p=0.0020; risk ratio 0.15, 95% CI 0.04–0.61), demonstrating a 85% reduction in reintervention with EUS-GE.
– Stent patency duration: No significant difference was observed between groups.
– Gastric outlet obstruction scores: At 1 month, mean GOOS was significantly higher in the EUS-GE group (2.41, SD 0.7) than the duodenal stenting group (1.91, SD 0.9), p=0.012, indicating better oral intake.
– Technical and clinical success: Both interventions had comparable technical success rates and clinical improvements.
– Mortality and safety: Deaths within 30 days were not statistically different (21% EUS-GE vs. 12% stenting, p=0.286). Adverse events within 30 days occurred in 23% and 24% of patients in EUS-GE and stenting groups respectively (p=1.00). Procedure-related pneumonia was reported in two EUS-GE patients and one stenting patient.
– Quality of life: No significant differences at 1 month between groups.
Expert Commentary
The DRA-GOO trial provides robust evidence supporting EUS-GE as an effective and safe alternative to conventional uncovered duodenal stenting for palliation of malignant gastric outlet obstruction. The significantly lower reintervention rate with EUS-GE reflects the mechanical advantage of bypassing the obstructing lesion, reducing tumor-related stent restenosis or migration risks. Improved 1-month GOOS further confirms patient-centered benefits in oral intake.
Importantly, the comparable safety profile and technical success affirm the feasibility of EUS-GE in expert centers. While 30-day mortality rates favored neither group significantly, longer-term survival remains limited by the underlying advanced malignancy.
Potential limitations include the necessity of specialized endoscopic expertise and equipment for EUS-GE, which may restrict widespread adoption. Additionally, the trial population reflects tertiary referral center patients and may not generalize to all clinical settings. Ongoing efforts to standardize EUS-GE techniques and device innovations are anticipated to improve accessibility and outcomes.
Conclusion
For patients suffering from malignant gastric outlet obstruction due to unresectable primary malignancies, endoscopic ultrasonography-guided gastroenterostomy offers a significantly reduced need for reintervention and better restoration of oral intake compared with uncovered duodenal metal stenting. The comparable safety and technical success endorse EUS-GE as a preferred palliative modality when resources and expertise are available. Future studies could focus on cost-effectiveness, long-term survival, and quality-of-life trajectories to optimize patient-centered care pathways.
References
Teoh AYB, Lakhtakia S, Tarantino I, Perez-Miranda M, Kunda R, Maluf-Filho F, Dhir V, Basha J, Chan SM, Ligresti D, Ma MTW, de la Serna-Higuera C, Yip HC, Ng EKW, Chiu PWY, Itoi T. Endoscopic ultrasonography-guided gastroenterostomy versus uncovered duodenal metal stenting for unresectable malignant gastric outlet obstruction (DRA-GOO): a multicentre randomised controlled trial. Lancet Gastroenterol Hepatol. 2025 Jun;10(6):e8-e16. doi: 10.1016/S2468-1253(25)00136-0. PMID: 40347959.