Highlight
- After valve-in-valve transcatheter aortic valve implantation (TAVI), dual antiplatelet therapy (DAPT) may reduce the risk of stroke compared to single antiplatelet therapy (SAPT).
- No significant differences were observed between DAPT and SAPT regarding major adverse cardiac and cerebrovascular events, major bleeding, or mortality within one year.
- Structural valve deterioration rates were low and similar between treatment strategies at one-year follow-up.
Study Background
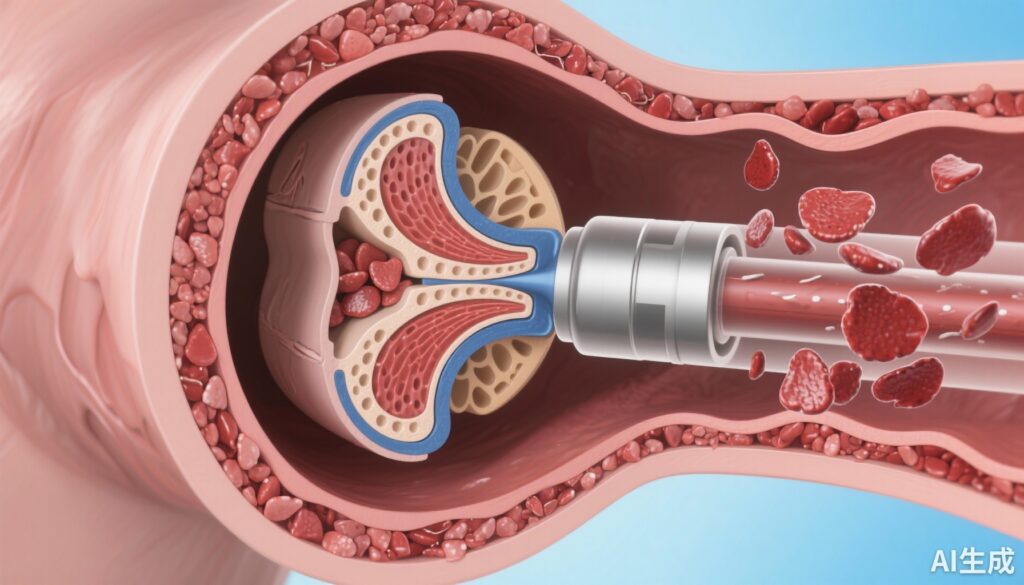
Transcatheter aortic valve implantation (TAVI) has become a well-established therapeutic option for patients with severe aortic stenosis, especially those at high or intermediate surgical risk. Single antiplatelet therapy (SAPT) is routinely recommended post-TAVI to reduce thrombotic complications. However, valve-in-valve TAVI, wherein a transcatheter valve is deployed within a failing surgical bioprosthesis, presents distinct challenges. This procedure may carry an elevated thrombogenic risk due to altered valve hemodynamics and increased tissue interface, potentially warranting more aggressive antithrombotic strategies. Despite this theoretical rationale, the optimal antiplatelet regimen following valve-in-valve TAVI remains unclear, as intensified therapy could increase bleeding risks without clear ischemic benefit. This study aimed to evaluate the comparative efficacy and safety of dual versus single antiplatelet therapy after valve-in-valve TAVI during the first post-procedure year.
Study Design
This multicenter cohort study included 278 patients undergoing valve-in-valve TAVI at 10 participating centers. Patients were grouped based on antiplatelet regimens received post-procedure: dual antiplatelet therapy (DAPT) or single antiplatelet therapy (SAPT). Patients receiving oral anticoagulants were excluded to isolate the effect of antiplatelet strategies. Clinical outcomes including major adverse cardiac and cerebrovascular events (MACCE), stroke incidence, major bleeding events, all-cause mortality, and echocardiographic assessment of structural valve deterioration were collected and analyzed at 12 months. To control for confounding factors, a propensity score was calculated, and inverse probability of treatment weighting was applied when estimating hazard ratios (HRs).
Key Findings
The study population comprised 278 patients, with comparable baseline demographics and procedural characteristics after propensity adjustment. The primary findings were as follows:
– No statistically significant difference was found between DAPT and SAPT groups for the composite endpoint of MACCE (HR 0.499; 95% confidence interval [CI], 0.182–1.371; P=0.178).
– Major bleeding events occurred at similar rates with HR 0.776 (95% CI, 0.172–3.504; P=0.741), indicating no significant bleeding risk increase with DAPT.
– All-cause mortality at one-year follow-up did not significantly differ between groups (HR 0.907; 95% CI, 0.272–3.022; P=0.874).
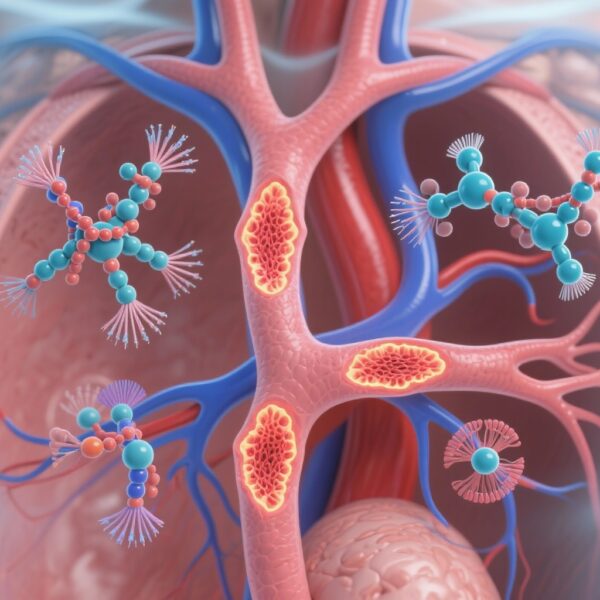
– Notably, stroke incidence was significantly lower in the DAPT cohort (HR 0.093; 95% CI, 0.010–0.831; P=0.033), suggesting a protective effect of dual therapy against cerebrovascular events.
– Echocardiographic evaluations showed low rates of moderate or severe structural valve deterioration in both groups (1.9% in DAPT vs 6.0% in SAPT, P=0.161), without statistically significant differences.

Expert Commentary
This observational study addresses an important clinical question in post-valve-in-valve TAVI management, highlighting a potentially favorable stroke risk reduction with DAPT without an increase in bleeding or mortality. The protective effect on stroke aligns biologically with intensified platelet inhibition reducing thromboembolic events arising from prosthetic valve surfaces or altered blood flow dynamics within a failing bioprosthesis. Nevertheless, the lack of significant differences in composite cardiovascular outcomes and valve deterioration suggests that benefits might be narrowly focused on cerebrovascular event prevention.
However, the study has intrinsic limitations. Its observational design precludes causal inference, and residual confounding despite propensity adjustment cannot be excluded. The relatively low event rates and one-year follow-up restrict assessment of longer-term valve durability and safety. Furthermore, exclusion of patients on oral anticoagulants, who commonly represent a higher thrombotic risk subgroup, limits generalizability.
Current guidelines emphasize individualized antithrombotic strategies post-TAVI, balancing ischemic and bleeding risks. This study supports consideration of DAPT early after valve-in-valve procedures to reduce stroke, yet randomized trials are needed to confirm these findings and to establish optimal duration and regimen of therapy.
Conclusion
In patients undergoing valve-in-valve TAVI for bioprosthetic valve failure, dual antiplatelet therapy may confer a significant reduction in one-year stroke risk compared to single antiplatelet therapy, without increased major bleeding, mortality, or valve deterioration. These findings suggest that a more intensive antiplatelet approach could improve cerebrovascular outcomes in this high-risk population. Nonetheless, further randomized controlled studies with longer follow-up are essential to validate these results, refine antiplatelet strategies, and optimize clinical practice.
Funding and Clinical Information
Funding details were not specified in the available data. This study was conducted across 10 centers as part of a collaborative clinical research effort. No clinical trial registration identifier was mentioned.
References
- Jaffe R, et al. Dual Versus Single Antiplatelet Therapy After Transcatheter Aortic Valve Implantation for Bioprosthetic Valve Failure. J Am Coll Cardiol Intv. 2025; DOI:10.1016/j.jcin.2025.09.018 IF: 11.4 Q1 .
- Kappetein AP, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: The Valve Academic Research Consortium-2 consensus document. Eur Heart J. 2013;34(31): 2383-2392.
- Valgimigli M, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease. Eur Heart J. 2018;39(3):213-260.