Study Background and Disease Burden
Obesity is a major global public health challenge, associated with increased morbidity and mortality due to its link to cardiometabolic diseases, type 2 diabetes, and certain cancers. Managing energy intake and appetite is central to obesity treatment strategies. Gut-derived hormones such as cholecystokinin (CCK), glucagon-like peptide-1 (GLP-1), and peptide tyrosine-tyrosine (PYY) are critical regulators of satiety, gastric emptying, and energy homeostasis. Nutritional interventions that modulate these gut hormones have shown promise in appetite control. L-tryptophan (Trp), an essential amino acid, has anorexigenic properties mediated partly by releasing these satiety hormones. Prior research in lean male individuals demonstrated that intraduodenal calcium enhances the suppressive effects of Trp on energy intake, implicating calcium’s role in gut hormone modulation. However, this interaction’s efficacy and dose-dependence in individuals with obesity, who often exhibit altered gut hormone responses, remains poorly understood. Elucidating these mechanisms is essential to explore novel, safe strategies to augment appetite regulation in obesity management.
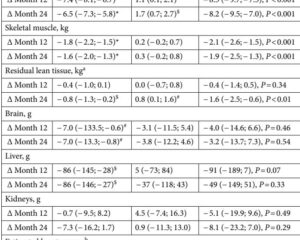
Study Design
This randomized, double-blind, crossover study enrolled fifteen males with obesity (mean ± SD: age 27 ± 8 years; BMI 30 ± 2 kg/m2; HbA1c 5.3 ± 0.2%) without type 2 diabetes. Participants underwent three separate experimental sessions during which they received 150-minute intraduodenal infusions consisting of three varying calcium doses (0 mg, 500 mg, or 1000 mg), each combined with a submaximal dose of L-tryptophan (load: 0.1 kcal/min) delivered from 75 to 150 minutes. Biochemical endpoints included plasma concentrations of gut hormones—gastrin, CCK, glucose-dependent insulinotropic polypeptide (GIP), GLP-1, and PYY—as well as measurements of antropyloroduodenal motility through pyloric pressure recordings. Immediately following infusions (150-180 minutes), energy intake was assessed at a standardized buffet-style lunch to quantify functional appetite suppression.
Key Findings
The administration of intraduodenal calcium at 1000 mg alone significantly stimulated plasma GLP-1 and PYY concentrations and increased pyloric motility pressures (all p < 0.05), without affecting gastrin or GIP. When combined with L-tryptophan, calcium enhanced the secretion of CCK, GLP-1, and PYY significantly compared to Trp alone (p < 0.05 for all). This hormonal potentiation correlated with a dose-related suppression of energy intake postinfusion, with calcium doses inversely associated with calorie consumption (r = -0.64; p = 0.001). Additionally, plasma CCK (r = 0.44; p = 0.05), GLP-1 (r = 0.60; p = 0.01), and PYY (r = 0.83; p = 0.01) concentrations correlated positively with calcium dose.
No significant changes were observed in gastrin or GIP levels, highlighting a selective modulatory effect restricted to key anorexigenic hormones. The observed increase in pyloric pressure suggests enhanced regulation of gastric emptying, further contributing to appetite suppression.
Safety parameters were not explicitly detailed in the study, but no adverse effects were reported, consistent with calcium doses within dietary supplementation ranges.
Expert Commentary
This study offers compelling evidence that intraduodenal calcium administration amplifies the gut hormone-mediated anorexigenic effects of L-tryptophan in males with obesity. The augmentation of CCK, GLP-1, and PYY—a triad central to satiety signaling and gastric motility regulation—advances our understanding of dietary macronutrient and mineral interplay in appetite control mechanisms. The dose-dependent effects underscore calcium’s potential as a strategic adjuvant to enhance amino acid-induced satiety responses in obesity.
Mechanistically, calcium sensing in the gut lumen is mediated by the calcium-sensing receptor (CaSR), which activates enteroendocrine cells to release these hormones. Enhanced pyloric pressure may slow gastric emptying, prolonging nutrient exposure to distal gut segments, further potentiating hormone secretion and satiety signaling.
Limitations include the small, exclusively male participant cohort, limiting generalizability to females and other populations. The study also focused exclusively on intraduodenal infusion rather than oral supplementation, which may differ in bioavailability and physiological impact. Potential long-term effects and safety of chronic calcium administration in combination with amino acid substrates warrant further investigation.
Moreover, the lack of effect on gastrin and GIP suggests specificity within gut hormone pathways, which could inform targeted nutritional approaches avoiding perturbation of glucose metabolism.
Conclusion
Intraduodenal administration of calcium at doses up to 1000 mg enhances L-tryptophan-induced secretion of the satiety hormones CCK, GLP-1, and PYY and concomitantly suppresses short-term energy intake in males with obesity. These findings provide a promising foundation for leveraging calcium as a modifiable dietary factor to augment amino acid-mediated appetite regulation.
Future research should explore oral delivery methods, long-term clinical outcomes, and broader population applicability to translate these mechanistic insights into practical interventions for obesity management.
References
1. Anjom-Shoae J, Fitzgerald PCE, Horowitz M, Holst JJ, Rehfeld JF, Veedfald S, Feinle-Bisset C. Dose-related Effects of Calcium to Enhance the Effects of L-tryptophan on Gut Hormones and Energy Intake in Obesity. J Clin Endocrinol Metab. 2025 Aug 7;110(9):e2929-e2938. doi: 10.1210/clinem/dgaf008. PMID: 39785828; PMCID: PMC12342367.
2. Pilichiewicz AN, et al. Influence of protein and fat on gut hormones and energy intake in obesity. Obesity (Silver Spring). 2016;24(3):561-569.
3. Batterham RL, et al. Gut hormone modulation to treat obesity and diabetes. Lancet Diabetes Endocrinol. 2020;8(3):192-202.
4. Camilleri M. Peripheral mechanisms in appetite regulation during obesity and diabetes: regulatory peptides, gut motility, and central nervous system responses. Gastroenterology. 2015;148(6):1145-1158.