Highlight
- Digital asthma self-management (DASM) significantly improved symptom control in adults with uncontrolled asthma compared to usual care.
- The intervention’s efficacy was notably lower among African American participants, highlighting persistent health disparities.
- Patient-reported outcomes and medication adherence also improved with the DASM intervention.
- Consistent symptom logging was associated with better outcomes, but engagement varied by race.
Background
Asthma remains a chronic respiratory disease with substantial morbidity, affecting over 25 million Americans and leading to over 1.6 million emergency department visits annually. Despite advances in pharmacotherapy and guideline-based care, a large proportion of adults continue to experience suboptimal symptom control. Self-management—encompassing medication adherence, symptom monitoring, and timely response to exacerbations—is foundational to asthma care, yet barriers persist, especially among racial and ethnic minorities. The rise of digital health tools offers a promising avenue to enhance self-management, potentially bridging gaps in care delivery and patient engagement.
Study Overview and Methodological Design
Silberman et al. conducted a randomized clinical trial to evaluate the effectiveness of a digital asthma self-management (DASM) program in adults. The study enrolled 899 adults (mean age 36.6 years, 71.1% women) with a predominance (61.3%) of uncontrolled asthma. Participants were recruited via email between October 2020 and November 2021. The population was randomly assigned to receive either the DASM intervention (n=450) or usual care (n=449). All participants installed a custom smartphone app and used wearable devices to support data collection.
The DASM intervention group received a comprehensive digital self-management tool featuring symptom tracking, alerts, and educational components. The control group accessed a limited version, restricted to the asthma control test and survey data collection. The primary endpoint was the 12-month change in asthma control test (ACT) scores, where scores ≤19 indicate uncontrolled asthma. Secondary outcomes included rates of symptom logging and patient-reported outcomes such as medication adherence, self-efficacy, readiness to change, and work productivity.
Key Findings
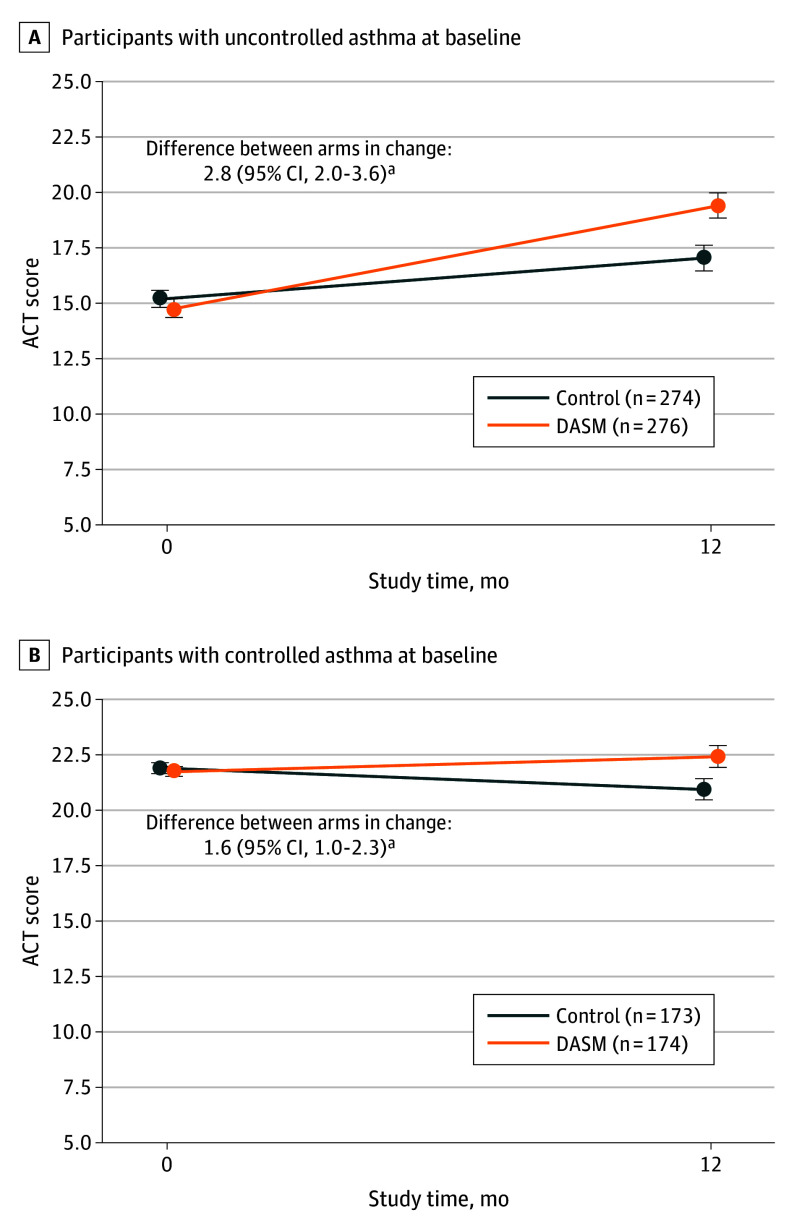
Among those with uncontrolled asthma at baseline, the DASM group achieved a mean improvement of 4.6 points on the ACT at 12 months, compared to a 1.8-point improvement in the usual care group. The adjusted between-group difference was 2.8 points (P < .001), considered both statistically and clinically significant.
Figure . Change in Asthma Control Test (ACT) Score by Arm and Baseline Asthma Control Status.
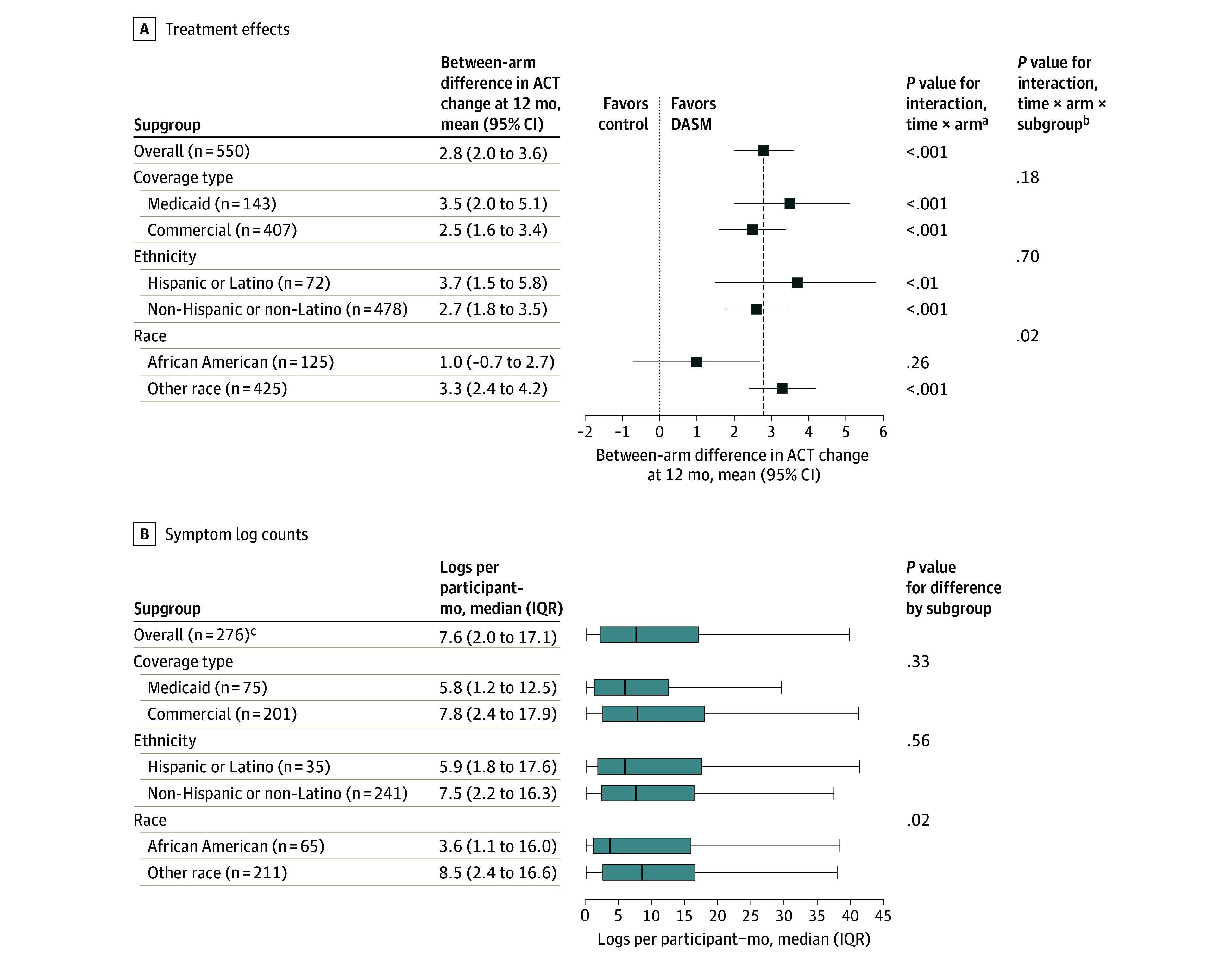
However, the treatment effect varied by race. African American participants demonstrated a non-significant 1.0-point improvement (P = .26) compared to a robust 3.3-point improvement (P < .001) in non-African American participants. Symptom logging rates were similar across insurance types and ethnicities, but African American participants logged symptoms less frequently than their counterparts.
Patient-reported outcomes further supported the DASM’s benefits: participants in the intervention group reported higher medication adherence, greater readiness to change self-management behaviors, increased confidence in managing their health, and reduced asthma-related work productivity impairment (P ≤ .001 for all measures).
Figure 4. Treatment Effects and Symptom Log Counts by Subgroup.
Clinical Implications
For clinicians, this study underscores the potential of digital self-management programs to improve asthma control, particularly in tech-savvy adult populations with uncontrolled symptoms. Integration of such tools into routine care could reduce exacerbations, enhance medication adherence, and improve quality of life. However, the differential effect across racial groups highlights the need for culturally tailored digital interventions. Clinicians should be vigilant in evaluating patient engagement and addressing barriers to technology use—especially in populations historically affected by health disparities.
Limitations and Controversies
Key limitations include the study’s reliance on self-reported outcomes, which may be subject to recall or reporting bias. The digital intervention’s effectiveness may not generalize to populations with limited digital access or literacy. The study sample, recruited via email, may overrepresent digitally engaged individuals. The weaker results among African American participants raise questions about the intervention’s equity and the need for deeper qualitative research to identify modifiable barriers.
Expert Commentary or Guideline Positioning
Current asthma management guidelines (e.g., GINA, NHLBI) advocate for individualized self-management plans, including digital tools when appropriate. This study supports incorporating DASM solutions as an adjunct to standard care, but also signals the necessity for equity-focused design and implementation. In an editorial accompanying the study, experts have called for co-creation of digital health tools with community input to maximize reach and effectiveness in underserved groups (GINA 2024, NHLBI 2022).
Conclusion
Digital asthma self-management programs can meaningfully improve symptom control and patient-reported outcomes in adults, but their benefits are not uniformly distributed. Addressing racial disparities in engagement and outcomes will be crucial as digital health becomes increasingly central to chronic disease management. Ongoing and future research should prioritize inclusive design strategies and robust implementation science to ensure that digital health innovation translates into equitable clinical benefit.
References
1. Silberman J, Sarlati S, Harris B, et al. A Digital Asthma Self-Management Program for Adults: A Randomized Clinical Trial. JAMA Netw Open. 2025;8(7):e2521438. doi:10.1001/jamanetworkopen.2025.21438 IF: 9.7 Q1 .2. Global Initiative for Asthma (GINA). Global Strategy for Asthma Management and Prevention, 2024 Update. https://ginasthma.org/
3. National Heart, Lung, and Blood Institute (NHLBI). 2022 Focused Updates to the Asthma Management Guidelines. https://www.nhlbi.nih.gov/health-topics/asthma
4. Pew Research Center. Mobile Technology and Home Broadband 2021. https://www.pewresearch.org/internet/2021/06/22/mobile-technology-and-home-broadband-2021/