Highlight
– DB-OTO gene therapy demonstrated significant hearing restoration in children with profound hearing loss due to OTOF mutations.
– After a single intracochlear infusion, 75% of participants reached clinically meaningful hearing thresholds, enabling natural acoustic hearing.
– The therapy was well tolerated, with no treatment discontinuations despite some adverse events.
– DB-OTO holds potential to reduce or eliminate the need for cochlear implants in affected patients, representing a major advance in inherited deafness treatment.
Study Background
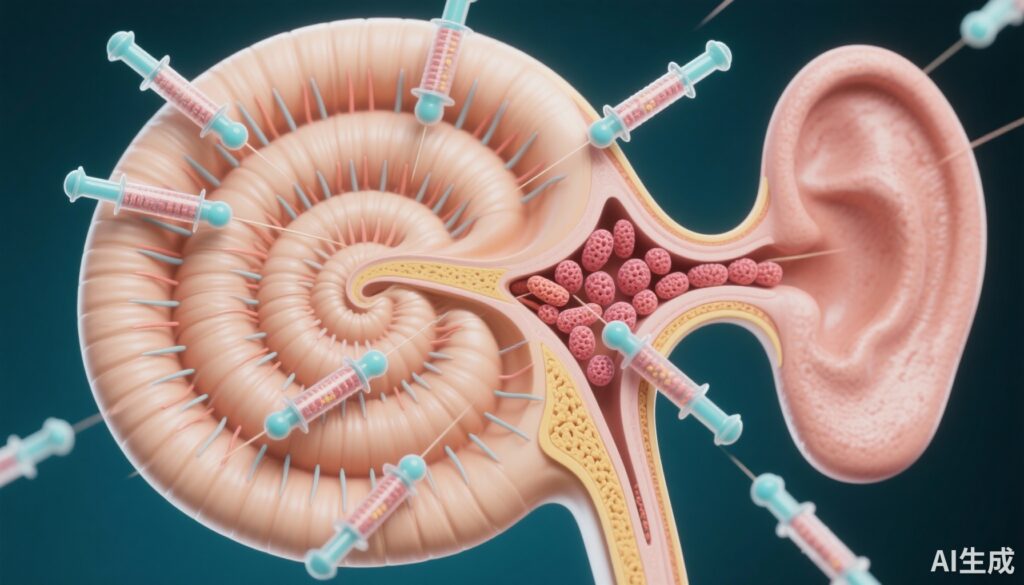
Inherited hearing loss caused by mutations in the OTOF gene leads to profound congenital deafness, severely impacting communication and quality of life in affected children. The OTOF gene encodes otoferlin, a protein critical for synaptic vesicle release in inner hair cells of the cochlea, necessary for auditory signal transmission to the brain. Defects in otoferlin disrupt this synaptic mechanism, resulting in auditory neuropathy and profound hearing impairment.
Traditional interventions, such as cochlear implants, can partially restore hearing but involve invasive surgery and do not replicate natural acoustic hearing. Gene therapy offers the promise of addressing the underlying genetic defect, potentially restoring physiological hearing function. However, safe and effective gene delivery to cochlear hair cells has posed significant challenges.
DB-OTO is a novel adeno-associated virus (AAV)-based gene therapy designed to deliver a functional copy of the OTOF gene selectively to cochlear hair cells, aiming to restore otoferlin expression and synaptic function. It has already received orphan drug, rare pediatric disease, and fast track designations from the FDA, underscoring its potential to address this unmet medical need.
Study Design
Regeneron conducted an open-label, single-arm, first-in-human registrational study to evaluate the safety and efficacy of DB-OTO in pediatric patients with genetically confirmed OTOF variants and profound deafness, defined as an average pure-tone audiometry threshold exceeding 90 decibel hearing level (dB HL).
Twelve children received a single intracochlear infusion of DB-OTO at a dose of 7.2×10^12 vector genomes per ear, administered unilaterally or bilaterally.
The primary efficacy endpoint was achieving an average pure-tone audiometry threshold of 70 dB HL or less at 24 weeks post-treatment, a clinical benchmark associated with hearing preservation that typically avoids cochlear implantation and supports natural acoustic hearing.
A key secondary endpoint was the presence of an auditory brain-stem response to click stimuli at or below 90 dB normalized hearing level (dB nHL) at 24 weeks, indicating functional auditory nerve and brainstem pathway activation. Safety assessments included monitoring adverse events, laboratory parameters, and vestibular function testing.
Key Findings
Of the 12 enrolled children treated with DB-OTO, nine (75%; 95% CI, 43 to 95) met both primary and secondary endpoints at 24 weeks after a single infusion, demonstrating statistically significant improvement (P = 1.1×10^-13).
These nine participants achieved a behavioral pure-tone average hearing threshold of 70 dB HL or less, indicating a shift from profound deafness to functional hearing levels amenable to verbal communication without invasive devices. Among them, six children attained the ability to hear soft speech without assistive devices, and notably, three patients exhibited near-normal average hearing sensitivity, highlighting the therapy’s potential to normalize auditory function.
Auditory brainstem responses corroborated these functional improvements, with thresholds improving to 90 dB nHL or better, underscoring restoration of auditory pathway integrity.
A total of 67 adverse events were recorded or worsened during or after treatment but were generally mild to moderate, with no participants withdrawing due to safety concerns. Adverse events did not indicate unexpected safety signals. Vestibular testing did not reveal clinically significant dysfunction associated with the intervention.
These robust efficacy and safety findings represent some of the first human data supporting AAV-mediated gene therapy for hereditary hearing loss caused by synaptic gene defects.
Expert Commentary
The CHORD Study Group’s publication in the New England Journal of Medicine marks a milestone in translational otology, demonstrating that ocular delivery of a functional gene to cochlear hair cells can meaningfully restore hearing in a previously untreatable genetic condition.
While the open-label, uncontrolled study design limits direct comparison to historical controls, the magnitude of hearing restoration and statistical significance are compelling. The ability to avoid cochlear implantation could reduce surgical risks, device-related complications, and lifelong technological dependence.
Future studies will need to assess durability of response beyond 24 weeks, efficacy across a broader age range and genetic variants, and long-term safety, including immune responses to the viral vector. Larger randomized trials will be essential for regulatory approval and clinical translation.
Mechanistically, restoring otoferlin addresses the fundamental synaptic transmission defect, providing biological plausibility for the observed functional gains. This represents a paradigm shift from symptomatic to disease-modifying therapy in inherited auditory neuropathies.
Conclusion
DB-OTO gene therapy offers a promising new avenue for treating congenital profound deafness due to OTOF gene mutations, with the potential to restore natural hearing and avoid cochlear implants. In this pioneering first-in-human study, 75% of treated children achieved clinically meaningful hearing improvement, including some with near-normal hearing thresholds, after a single treatment.
These results support ongoing clinical development and regulatory submissions planned by Regeneron Pharmaceuticals. The ongoing evolution of gene therapy for hereditary deafness holds transformative potential to improve communication and quality of life for affected children worldwide.
Further research will clarify long-term benefits, optimize dosing strategies, and expand indications to more genetic etiologies of hearing loss.
Funding and ClinicalTrial.gov
This study was funded by Regeneron Pharmaceuticals.
ClinicalTrials.gov identifier: NCT05788536.
References
Valayannopoulos V, Bance M, Carvalho DS, Greinwald JH Jr, Harvey SA, Ishiyama A, Landry EC, Löwenheim H, Lustig LR, Manrique M, Nash R, Polo R, Pritchett CV, Rubinstein JT, Shearer AE, Del Castillo I, Anderson JJ, Corrales CE, Quigley TM, Riggs WJ, Weber P, Wilson G, Irvin SC, Hassan HE, Chen Y, Liu R, Drummond MC, Sabin LR, Musser BJ, Yancopoulos GD, Kyratsous CA, Herman GA, Baras A, Whitton JP; CHORD Study Group. DB-OTO Gene Therapy for Inherited Deafness. N Engl J Med. 2025 Oct 12. doi: 10.1056/NEJMoa2400521. Epub ahead of print. PMID: 41085057.