Background
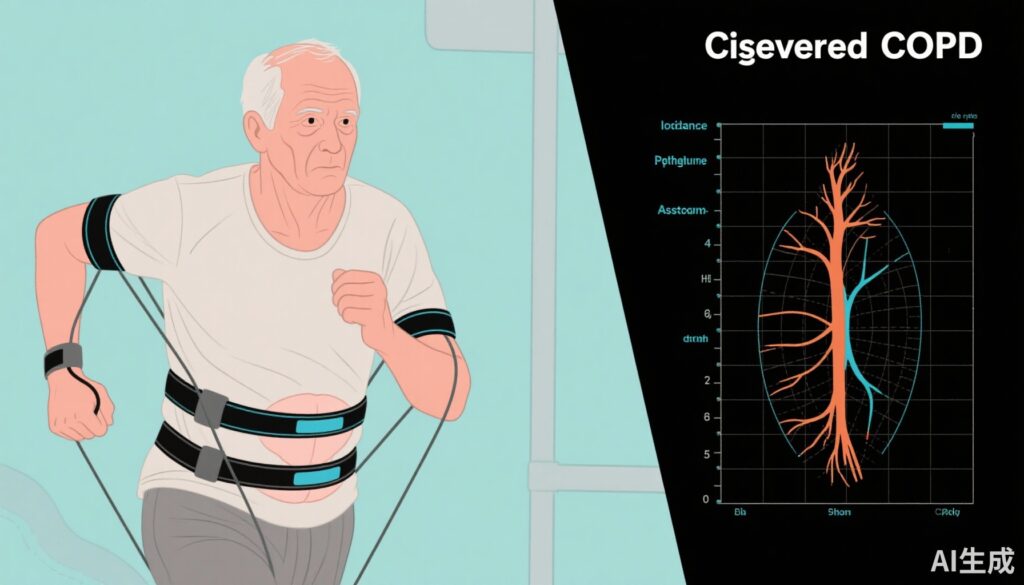
Chronic obstructive pulmonary disease (COPD) represents a heterogeneous condition hallmarked by persistent airflow limitation, chronic cough, sputum production, and episodic exacerbations. Chronic bronchitis, characterized by prolonged productive cough, is a prevalent COPD phenotype associated with excess mucus production and airway mucus plugging. Such plugging correlates with accelerated lung function decline, greater exacerbation risk, and increased mortality, yet remains an under-recognized challenge in COPD management. Despite polypharmacy with inhaled corticosteroids (ICS), long-acting beta-agonists (LABA), and muscarinic antagonists (LAMA), acute exacerbations of COPD (AECOPD) persist in up to 60% of patients, underlining an unmet therapeutic need.
Interleukin-33 (IL-33) has emerged as a potential pathogenic mediator in COPD, operating through both the ST2 and RAGE/EGFR signaling pathways. Monoclonal antibodies targeting IL-33 or its receptor ST2, such as itepekimab and astegolimab, have demonstrated preliminary efficacy signals in COPD subgroups defined by blood eosinophil count (BEC) or smoking status. Tozorakimab is a novel anti-IL-33 human monoclonal antibody that neutralizes both reduced IL-33 (IL-33^red) via ST2 and oxidized IL-33 (IL-33^ox) through RAGE/EGFR pathways, potentially addressing both inflammatory and mucus hypersecretion components.
Study Design
FRONTIER-4 (NCT04631016) was a randomized, double-blind, placebo-controlled phase 2a trial conducted across multiple international centers. The study enrolled 135 adults aged 40–80 years with moderate-to-severe COPD, chronic bronchitis, and a smoking history ≥10 pack-years. Eligible patients were on stable dual or triple inhaled maintenance therapy. Participants were randomized 1:1 to receive subcutaneous tozorakimab 600 mg or placebo every four weeks for 24 weeks.
The primary endpoint was the change from baseline to week 12 in pre-bronchodilator forced expiratory volume in 1 second (FEV1). Secondary outcomes included changes in post-bronchodilator FEV1, time-to-first composite COPD exacerbation event (COPDCompEx), patient-reported outcomes (PROs), safety, pharmacokinetics, and biomarkers. Predefined subgroup analyses assessed outcomes by exacerbation history (≥2 vs. ≤1 exacerbation in prior 12 months), baseline BEC (<150 vs. ≥150 cells/µL), and smoking status (current vs. former smokers).
Key Findings
In the intent-to-treat population (tozorakimab, n=67; placebo, n=68), tozorakimab elicited a nonsignificant 24 mL LS mean difference (80% CI -15 to 63 mL; p=0.216) increase in pre-bronchodilator FEV1 at week 12 compared to placebo. Importantly, a significant improvement was observed in post-bronchodilator FEV1 (67 mL; 80% CI 17–116 mL; p=0.044), sustained through week 28.

In the prespecified subgroup with ≥2 prior AECOPD, tozorakimab demonstrated larger improvements: 69 mL increase in pre-bronchodilator FEV1 (80% CI 9–130 mL; p=0.072) and 124 mL increase in post-bronchodilator FEV1 (80% CI 47–201 mL; p=0.020) versus placebo. Similar trends were noted in a post hoc-defined population with ≥2 moderate and/or ≥1 severe exacerbation history.
Regarding exacerbations, tozorakimab did not significantly reduce the risk of COPDCompEx events in the overall population (hazard ratio [HR] 0.79; 80% CI 0.57–1.11; p=0.186). However, a greater reduction in risk was observed among patients with ≥2 prior exacerbations (HR 0.61; 80% CI 0.37–1.00). No meaningful differences were noted based on BEC thresholds or smoking status.
Patient-reported respiratory symptom scores and health-related quality of life measures (SGRQ, E-RS, BCSS, cough VAS) showed no significant differences, consistent with the study’s limited power for these endpoints.

An exploratory CT sub-study (n=39) suggested that tozorakimab reduced mucus plugging in lung segments compared to placebo at week 28 (LS mean difference -1.5 segments; 80% CI -3.0 to 0.0; p=0.097), paralleling mechanistic data on mucus-producing cell modulation.
Biomarker analysis revealed that tozorakimab significantly reduced blood eosinophil counts by approximately 30%, along with decreases in IL-5, IL-13, and plasma fibrinogen levels, reinforcing its anti-inflammatory activity.

Safety data indicated that tozorakimab was generally well tolerated. The incidence of treatment-emergent adverse events (TEAEs) was similar between tozorakimab (79.1%) and placebo (73.5%) groups; most were mild or moderate. Injection-site erythema and headache were the most common adverse events related to tozorakimab. No deaths or life-threatening events were reported.
Expert Commentary
The FRONTIER-4 study offers valuable early-phase evidence on the dual anti-inflammatory and mucus-modulatory potential of tozorakimab in COPD patients with chronic bronchitis. The lack of statistically significant improvement in the primary endpoint of pre-bronchodilator FEV1 in the overall population may reflect the study’s limited size and heterogeneity. Nevertheless, the consistent efficacy signals in subgroups with higher exacerbation risk and elevated eosinophil counts align with earlier IL-33 pathway antibody trials and emphasize the importance of patient stratification.
The observed effects on mucus plugging, a key pathological feature linked to adverse outcomes, underscore tozorakimab’s novel mechanistic advantage in targeting oxidized IL-33-mediated RAGE/EGFR signaling. These findings are supported by biomarker reductions in type 2 inflammation markers. The similar efficacy between current and former smokers contrasts with prior studies suggesting differential responses, underscoring the need for larger trials to clarify the impact of smoking status.
Limitations include the COVID-19 pandemic’s interference with recruitment and exacerbation event ascertainment, underpowering for several endpoints, and the relatively short treatment duration. The use of a composite COPDCompEx endpoint also awaits further validation in larger cohorts.
Ongoing phase 3 trials (OBERON, TITANIA, MIRANDA, PROSPERO) with larger sample sizes and longer follow-up should clarify tozorakimab’s clinical utility, optimal patient selection, and potential to modify exacerbation risk and disease progression.
Conclusion
The phase 2a FRONTIER-4 trial demonstrated that although tozorakimab did not meet its primary endpoint in the overall COPD population, it provided encouraging efficacy signals in patients with a history of frequent exacerbations. Its dual mechanism targeting IL-33 pathways offers a promising therapeutic avenue for addressing inflammation and mucus hypersecretion in COPD. These findings warrant confirmation in ongoing larger studies to define tozorakimab’s role in COPD management.
References
Singh D, Guller P, Reid F, Doffman S, Seppälä U, Psallidas I, Moate R, Smith R, Kiraga J, Jimenez E, Brooks D, Kelly A, Nordenmark LH, Sadiq MW, Caballero LM, Kell C, Belvisi MG, Pandya H. A phase 2a trial of the IL-33 monoclonal antibody tozorakimab in patients with COPD: FRONTIER-4. Eur Respir J. 2025 Jul 14;66(1):2402231. doi: 10.1183/13993003.02231-2024 IF: 21.0 Q1 .