Introduction
Vascularized composite allotransplantation (VCA) has revolutionized reconstructive surgery by enabling the transplantation of complex tissues including skin, muscle, bone, and nerves. Despite successes, long-term graft survival remains challenged by chronic rejection (CR), which emerges as a predominant cause of late graft failure. Unlike traditional solid organ transplants, VCAs involve multiple tissue targets, leading to diverse CR types with unique clinical and pathological features. Understanding these manifestations, underlying mechanisms, and therapeutic avenues is critical to improve outcomes.
Clinical Manifestations of Chronic Rejection in VCA
Chronic rejection typically manifests several years post-transplantation, often presenting insidiously. Clinically, it involves progressive vascular narrowing (vasculopathy), skin changes, and loss of function in the grafted tissues.
In human VCA cases, skin atrophy, pigmentation changes, and telangiectasia may be observed. Vascular alterations such as vessel intimal hyperplasia lead to compromised blood flow, evidenced by ischemic changes and tissue necrosis. Adnexal structures, including hair follicles and sweat glands, may also be lost, contributing to the functional decline.
Animal models mirror these clinical features but allow detailed temporal analysis. They reveal that exposure to environmental insults accelerates CR, underscoring the role of external factors in disease progression.
Pathologic Features of Chronic Rejection
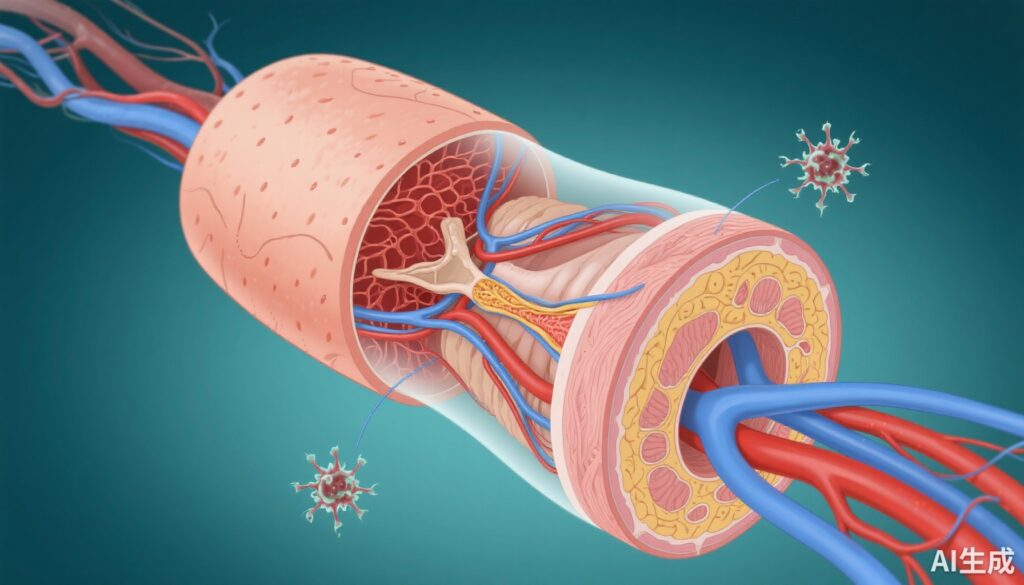
Pathologically, CR in VCA is characterized by vasculopathy, primarily intense intimal hyperplasia causing luminal narrowing. Other features include fibrosis of skin and soft tissues, loss of adnexal structures, and immune cell infiltration.
Vessel biopsies reveal thickened intima, proliferating smooth muscle cells, and deposition of immune complexes and complement components. Skin biopsies show epidermal thinning, dermal fibrosis, and diminished adnexal elements.
Based on these findings, a working classification distinguishes early vasculopathy with reversible changes from late, irreversible fibroproliferative stages.
Pathophysiology of Chronic Rejection
CR involves complex immune and non-immune mechanisms. Endothelial cell activation and injury play central roles, initiating inflammatory cascades that promote smooth muscle proliferation and fibrosis.
The process begins with alloimmune recognition involving T cells and antibodies, leading to complement activation and endothelial damage. Persistent immune responses, combined with environmental triggers like trauma, induce oxidative stress and cytokine release, fueling vascular remodeling.
Insights from diseases such as pulmonary arterial hypertension offer parallels; abnormal vasculature and proliferative mechanisms share similarities, suggesting common pathways such as growth factor signaling and oxidative stress.
Potential Targets and Interventions
Current and emerging strategies aim at modulating immune responses and protecting vasculature. Targeting complement pathways with inhibitors can reduce endothelial injury. Checkpoint inhibitors and immune tolerance induction hold promise to mitigate alloimmune activation.
Furthermore, therapies that inhibit vascular smooth muscle proliferation, such as tyrosine kinase inhibitors, are under investigation. Monitoring immune activity through biomarker development could enable early detection and intervention.
Prevention involves optimizing immunosuppressive regimens while minimizing side effects. Enhancing graft surveillance via non-invasive imaging and molecular diagnostics is vital for early CR detection.
Future Directions and Research Needs
Advancing our understanding of CR requires multidisciplinary research integrating immunology, vascular biology, and bioengineering. Developing sensitive, specific biomarkers for early detection, and improving targeted therapies, are critical. Additionally, exploring the role of environmental and mechanical factors in CR progression could unveil novel preventative strategies.
Innovations in gene editing and regenerative medicine may pave the way for durable, tolerance-inducing interventions. Ultimately, personalized approaches based on immune profiling could revolutionize long-term VCA management.
Conclusion
Chronic rejection remains a formidable barrier to the long-term success of VCA. Its complex interplay of immune, vascular, and environmental factors necessitates comprehensive strategies encompassing early detection, targeted immune modulation, and protective vascular therapies. Continued research guided by translational insights promises to improve graft longevity and patient quality of life.
References
1. Brandacher G, Messner F, Al-Salmay Y, Kaufman CL. Clinical Manifestation, Mechanisms, and Potential Targets of Intervention for Chronic Rejection in Vascularized Composite Allotransplantation. Transplantation. 2025 Nov 1;109(11):1710-1722. doi: 10.1097/TP.0000000000005450.
2. Welch, J. E., & Schlosser, R. J. (2022). Vasculopathy in transplantation: mechanisms and emerging therapies. Transplant Immunology, 65, 101434.
3. Smith, R. P., et al. (2021). Advances in biomarker development for chronic rejection. Transplantation Reviews, 35(4), 100661.
4. Perez, F. R., & Kwon, S. (2020). Mechanisms of vascular remodeling in transplant vasculopathy. Current Opinion in Organ Transplantation, 25(2), 218-225.
This comprehensive review underscores the multifaceted nature of CR in VCA and highlights avenues for innovative diagnostics and therapies, promising improved long-term graft survival and patient outcomes.