Highlights
- Adolescents within 10 days post-sport-related concussion exhibit symptom-limited exercise intolerance with increased perceived exertion despite no resting cardiopulmonary differences compared to controls.
- Elevated minute ventilation and early plateau of blood pressure during graded exercise, without evidence of aerobic deconditioning, suggest distinct cardiopulmonary response alterations in concussed youth.
- Graded aerobic exercise testing, including treadmill and cycle ergometer protocols, is safe and valuable for identifying physiological post-concussion dysfunction and guiding tailored exercise rehabilitation.
- Emerging evidence implicates autonomic nervous system dysregulation and altered cerebral blood flow control as underlying mechanisms of exercise intolerance and post-concussion syndrome.
Background
Sport-related concussion (SRC) remains a prevalent and clinically challenging injury in adolescent athletes, characterized by transient brain dysfunction following biomechanical forces to the head. Among the physiological sequelae of SRC, symptom-limited exercise intolerance is increasingly recognized as a key feature reflecting impaired systemic and central regulation of cardiopulmonary function rather than solely deconditioning. Traditional management emphasizing prolonged rest has come under scrutiny due to risk of aerobic deconditioning and delayed recovery. Understanding cardiopulmonary responses during graded exercise can clarify SRC pathophysiology and inform rehabilitation strategies aimed at optimizing safe return to activity.
Key Content
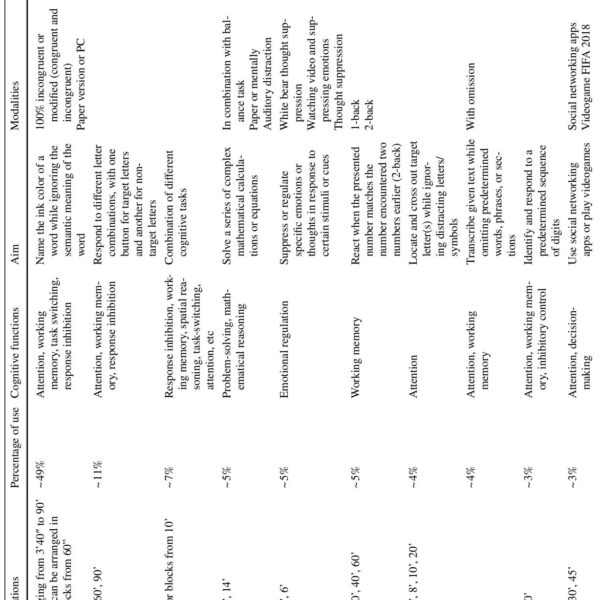
Chronological Development and Graded Exercise Testing Modalities
The clinical translation of graded aerobic exercise testing (GAET) in SRC pediatric populations dates back over a decade, with pivotal studies (e.g., Leddy et al., 2016) demonstrating safety and clinical utility of treadmill-based protocols to diagnose physiological post-concussion disorder (PCD) and tailor submaximal aerobic exercise prescriptions. The Buffalo Concussion Bike Test (BCBT), a progressive cycle ergometer test, represents a recent innovation providing detailed cardiopulmonary monitoring during exercise in concussed adolescents (Leddy JJ et al., 2025).
These protocols incrementally increase exercise intensity while continuously assessing heart rate (HR), blood pressure (BP), respiratory rate (RR), minute ventilation (VE), oxygen consumption (VO2), stroke volume (SV), cardiac output (CO), and end-tidal CO2 (PETCO2). The combination of subjective symptom reporting and objective physiological markers allows characterization of SRC-induced alterations and determination of individualized exercise thresholds.
Cardiovascular and Respiratory Responses in Adolescents After SRC
Recent evidence from the 2025 study by Leddy et al. involving adolescents within 10 days post-SRC (n=26) compared with matched controls (n=24) elucidated important cardiopulmonary differences during graded cycle exercise. Major findings include:
- No significant differences at rest in cardiovascular (HR, BP, SV, CO) or respiratory parameters (RR, VO2, PETCO2) between concussed and control groups, excluding early aerobic deconditioning.
- During exercise, concussed adolescents demonstrated a significantly higher minute ventilation relative to controls, suggestive of altered ventilatory control or compensatory mechanism to perceived metabolic demands.
- Blood pressure increases in concussed participants plateaued prematurely during the first 10 minutes of exercise, indicating possible impaired vascular or autonomic responsiveness impacting exercise tolerance.
- Concussed athletes exercised for a shorter time (16.24 ± 5.6 min) with exacerbation of concussion symptoms (≥2-point increase on a 0-10 scale) in their final minute, contrasted with controls who exercised longer (25.08 ± 7.0 min) without symptom provocation.
- Higher ratings of perceived exertion (RPE) during exercise were reported by concussed participants, reinforcing subjective exercise intolerance despite no evidence of deconditioning.
These findings align with those from other investigations using graded treadmill testing (Leddy et al., 2016) and cerebral blood flow assessments (Len et al., 2016), which collectively suggest that exercise intolerance post-SRC arises more from central autonomic dysregulation and altered neurovascular coupling than from peripheral cardiopulmonary deconditioning.
Mechanistic Insights and Autonomic Dysfunction Post-Concussion
The observed cardiopulmonary alterations implicate autonomic nervous system (ANS) dysfunction as a central mechanism. SRC can disrupt autonomic balance, resulting in impaired sympathetic and parasympathetic modulation of heart rate, blood pressure, and ventilatory control. Reduced sensitivity to CO2 and abnormal cerebral blood flow regulation contribute to exercise intolerance, as demonstrated by altered PETCO2 levels and cerebral blood flow velocity changes during graded exercise in PCS patients (Len et al., 2016).
Furthermore, muscle damage, physical exertion, and their interplay with neurological outcomes have been highlighted in subconcussive impacts studies (Baugh et al., 2020), signaling the need to consider systemic physiological stressors beyond the brain injury itself.
Clinical Implications and Rehabilitation Approaches
Graded aerobic exercise testing is emerging as a critical diagnostic and prognostic tool in pediatric SRC management, enabling differentiation of physiological from cervicogenic or migraine-related symptoms and guiding individualized submaximal exercise therapy. Evidence affirms the safety and utility of such testing within multidisciplinary concussion programs with high rates of symptom improvement and return-to-play success post-intervention (Leddy et al., 2016).
Impaired cardiopulmonary responses necessitate cautious exercise prescription to avoid premature symptom exacerbation, with gradual progression to full aerobic capacity during recovery. Understanding autonomic dysfunction enables potential integration of therapeutic strategies targeting ANS regulation, such as biofeedback, paced breathing, or pharmacotherapy, although such interventions require further clinical validation.
Expert Commentary
The collective literature underscores a paradigm shift from rest-centric management to active rehabilitation informed by dynamic physiological assessment. The Leddy et al. (2025) study fills a critical gap by demonstrating that within 10 days post-SRC, adolescent athletes do not manifest deconditioning per se but exhibit attenuated cardiovascular response and abnormal ventilatory patterns contributing to exercise intolerance.
Methodologically, continuous monitoring of cardiac output, stroke volume, and ventilatory parameters during cycle ergometer protocols offers granular data surpassing traditional treadmill assessments, allowing refined phenotyping of physiological impairments.
Limitations include small sample sizes and the need for longitudinal follow-up to delineate recovery trajectories and the impact of interventions. Additionally, potential sex differences and psychosocial factors warrant exploration.
Guidelines increasingly advocate for individualized exercise testing as a standard component of SRC care, emphasizing safety and symptom monitoring. Mechanistic understanding of autonomic dysregulation opens avenues for novel therapeutic targets and biomarker development to enhance recovery and prevent prolonged disability.
Conclusion
Recent evidence consolidates that adolescents sustaining sport-related concussion experience distinctive cardiopulmonary response alterations during graded exercise without concurrent aerobic deconditioning in the acute post-injury phase. Elevated ventilatory rates and early blood pressure plateau signify autonomic dysregulation contributing to symptom-limited exercise tolerance.
Clinical management benefits from incorporation of graded aerobic exercise testing for objective functional assessment and to tailor submaximal exercise rehabilitation protocols that promote recovery while mitigating symptom exacerbation. Further research should explore autonomic function, cerebrovascular regulation, and personalized therapeutic strategies to optimize return-to-play outcomes in this vulnerable population.
References
- Leddy JJ, Haider MN, Chizuk HM, Nazir MSZ, Worts P, Willer BS, Johnson BD. Cardiovascular and Respiratory Responses During Graded Exercise in Adolescents After Sport-Related Concussion. Sports Med. 2025 Aug 26. doi: 10.1007/s40279-025-02301-7. Epub ahead of print. PMID: 40858863.
- Leddy JJ, Baker JG, Kozlowski K, Bisson LJ, Willer BS. A Preliminary Study of the Effect of Subthreshold Aerobic Exercise on Symptoms Following Sport-Related Concussion in Pediatric Patients. Clin J Sport Med. 2016 Dec;25(6):471-477. doi: 10.1097/JSM.0000000000000306. PMID: 27620871.
- Len TK, Neary JP, Jean K, McCauley SR, Cook DB. Cerebral Blood Flow During Treadmill Exercise Is a Marker of Physiological Postconcussion Syndrome in Female Athletes. J Head Trauma Rehabil. 2016 May-Jun;31(3):215-24. doi: 10.1097/HTR.0000000000000145. PMID: 26098254.
- Baugh CM, Kroshus E, Daneshvar DH, Zhao C, Stern RA. Association between Muscle Damage and Head Impacts in High School American Football. Int J Sports Med. 2020 Jan;41(1):36-43. doi: 10.1055/a-1021-1735. PMID: 31747699.