Highlight
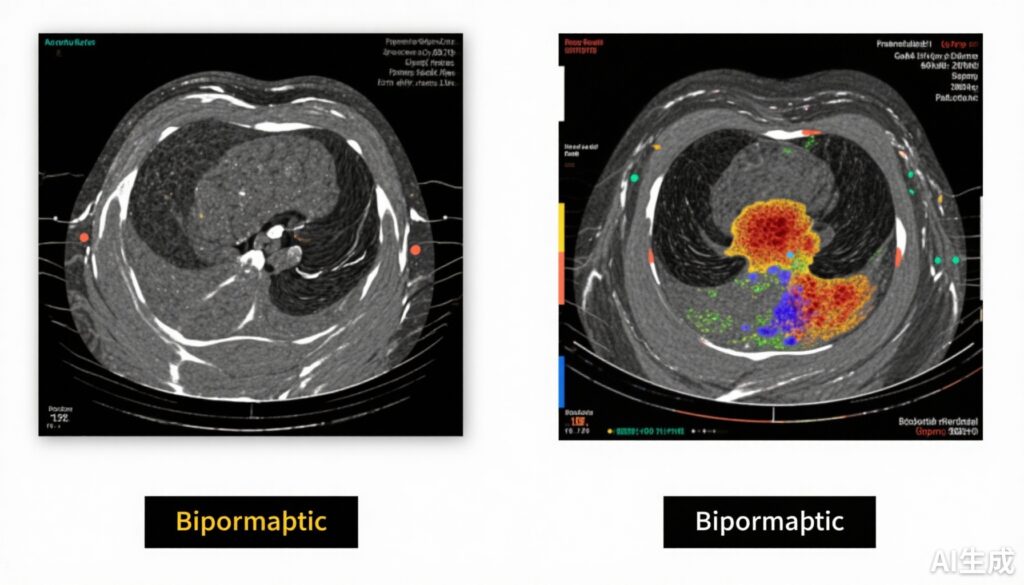
- Biparametric MRI (bpMRI), which excludes dynamic contrast-enhanced sequences, is noninferior to multiparametric MRI (mpMRI) in diagnosing clinically significant prostate cancer.
- The PRIME trial, a large-scale, multicenter prospective study involving 490 biopsy-naive men with suspected prostate cancer, confirmed bpMRI’s diagnostic accuracy closely matches mpMRI.
- Biparametric MRI offers substantial resource and time savings, potentially increasing global MRI throughput and reducing costs for prostate cancer diagnosis.
Study Background
Prostate cancer remains one of the most common malignancies among men worldwide, where early and accurate diagnosis of clinically significant prostate cancer is critical for appropriate treatment decisions. Currently, multiparametric magnetic resonance imaging (mpMRI) incorporating T2-weighted, diffusion-weighted, and dynamic contrast-enhanced (DCE) imaging sequences forms the diagnostic gold standard. This approach improves cancer detection accuracy and guides targeted biopsies, reducing unnecessary biopsies and overdiagnosis of clinically insignificant disease.
However, mpMRI is resource-intensive, requiring gadolinium-based contrast agents that add cost, extend scan time, and impose risks, particularly in patients with renal impairment. Health systems globally face challenges in meeting demand for mpMRI, which limits widespread accessibility. Biparametric MRI (bpMRI), which omits the DCE sequence and relies solely on T2-weighted and diffusion-weighted imaging, represents a potentially faster, cheaper alternative. Although previous smaller studies suggested comparable diagnostic performance, robust large-scale evidence has been lacking.
Study Design
The PRIME diagnostic clinical trial was a prospective, multicenter, within-patient noninferiority study conducted across 22 centers in 12 countries. It enrolled 555 biopsy-naive men with clinical suspicion of prostate cancer based on elevated prostate-specific antigen (PSA) levels and/or abnormal digital rectal exam findings between April 2022 and September 2023.
Each participant underwent mpMRI comprising T2-weighted, diffusion-weighted, and dynamic contrast-enhanced sequences. Radiologists initially interpreted the bpMRI component (T2-weighted and diffusion-weighted only) blinded to the DCE images before assessing the full mpMRI. Men with imaging findings suggestive of clinically significant prostate cancer on either bpMRI or mpMRI underwent targeted biopsy, with or without systematic biopsy.
The primary endpoint was the proportion of men diagnosed with clinically significant prostate cancer (generally defined as Grade Group 2 or higher). Secondary endpoints included detection rates of clinically insignificant cancer. The trial prespecified a noninferiority margin of 5%. Quality control confirmed diagnostic adequacy in 99% of scans.
Key Findings
Out of 490 evaluable men, the median age was 65 years and median PSA level was 5.6 ng/mL. Abnormal digital rectal exams were present in 12.7%.
Biparametric MRI detected clinically significant prostate cancer in 143 men (29.2%), nearly identical to mpMRI detection in 145 men (29.6%)—a negligible difference of -0.4 percentage points (95% CI: -1.2 to 0.4; P = 0.50) well within the predefined noninferiority threshold.
Detection of clinically insignificant cancer was also similar: 9.2% with bpMRI versus 9.6% with mpMRI (difference -0.4 percentage points; 95% CI: -1.2 to 0.4). This indicates bpMRI does not increase overdiagnosis.
Quality of imaging was high, with the vast majority of scans deemed diagnostically adequate, supporting the reliability of results across various centers.
Expert Commentary
The PRIME trial provides compelling high-level evidence that bpMRI matches mpMRI in detecting clinically significant prostate cancer while maintaining limitations on clinically insignificant tumor detection. Omitting DCE sequences reduces scan time, contrast agent use, and costs without compromising diagnostic accuracy.
Given the increasing global demand for prostate MRI, bpMRI adoption could alleviate scanner bottlenecks and enhance healthcare accessibility, especially in resource-constrained settings. This simplification aligns with emerging international guideline updates and expert consensus advocating streamlined imaging protocols when image quality is assured.
However, caution is warranted to ensure adequate radiologist expertise and image quality standards to maintain diagnostic performance. Certain clinical scenarios, such as post-treatment evaluation or comprehensive staging, may still require full mpMRI. Further research could refine patient selection criteria for bpMRI versus mpMRI.
Conclusion
The PRIME diagnostic trial confirms that biparametric MRI is noninferior to multiparametric MRI for diagnosing clinically significant prostate cancer in biopsy-naive men. This abbreviated imaging approach could become the new standard of care, improving diagnostic efficiency, reducing costs, and expanding global access to high-quality prostate cancer evaluation. Implementing bpMRI protocols requires attention to quality assurance and training but offers a promising pathway to optimize prostate cancer diagnostic workflows worldwide.
References
Ng ABCD, Asif A, Agarwal R, Panebianco V, Girometti R, Ghai S, Gómez-Gómez E, Budäus L, Barrett T, Radtke JP, et al; PRIME Study Group Collaborators. Biparametric vs Multiparametric MRI for Prostate Cancer Diagnosis: The PRIME Diagnostic Clinical Trial. JAMA. 2025 Oct 7;334(13):1170-1179. doi:10.1001/jama.2025.13722.
European Association of Urology. EAU Guidelines on Prostate Cancer 2024 Edition. Available at: https://uroweb.org/guidelines/prostate-cancer/
American Urological Association. Prostate Imaging and Biopsy Guidelines. 2023 Update.
Padhani AR, Barentsz J, Villeirs G, et al. PI-RADS v2.1: a critical update for prostate MRI interpretation. Radiology. 2019;292(2):464-474.