Highlight
- The BIOLAP trial is the first large, randomized, self-controlled study comparing biological and synthetic meshes in bilateral laparoendoscopic inguinal hernia repair.
- At 6 months postoperatively, there was no significant difference in patient-reported pain between biological and synthetic meshes.
- Biological meshes exhibited significantly higher 2-year hernia recurrence rates (11.2% vs 2.5%) and increased seroma formation (33.4% vs 21.6%) compared with synthetic meshes.
- These findings do not support switching from synthetic to biological meshes in routine laparoendoscopic inguinal hernia repair.
Study Background
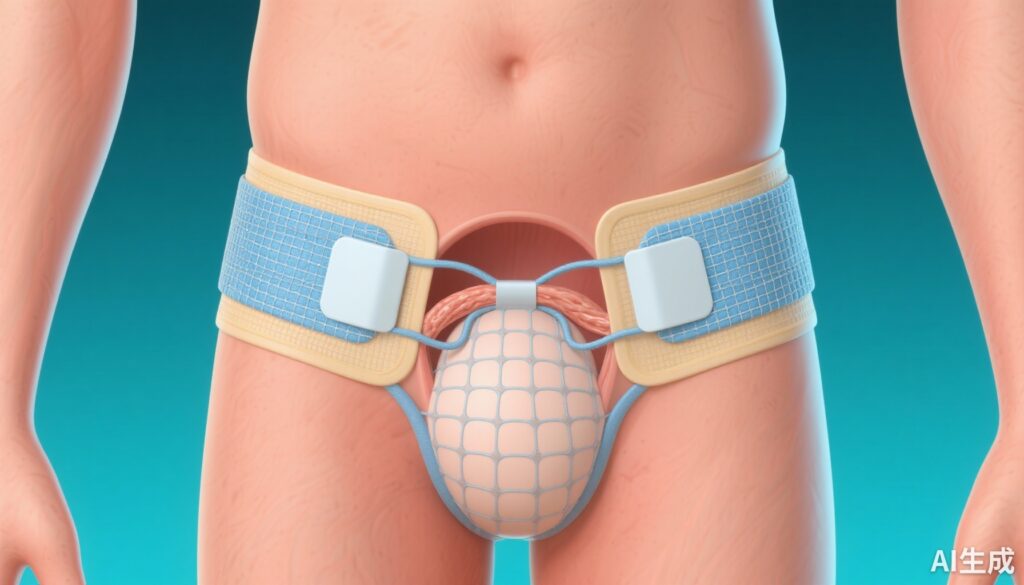
Inguinal hernia repair is one of the most commonly performed general surgical procedures worldwide. Despite advances in technique, chronic postoperative pain and hernia recurrence remain significant complications impacting patient quality of life and long-term outcomes. Synthetic mesh implants have been the standard choice to reinforce the inguinal floor, reducing recurrence risk, but concerns remain about chronic pain and foreign body reactions.
Biological meshes, derived from resorbable natural materials, have been proposed as alternatives that might reduce postoperative pain by minimizing chronic inflammatory responses. However, robust comparative data on outcomes such as pain, recurrence, and postoperative complications are lacking, especially in laparoendoscopic approaches where tension-free repair is feasible and mesh choice could influence results.
Study Design
The Biological vs Synthetic Mesh in Laparoendoscopic Inguinal Hernia Repair (BIOLAP) trial was a multicenter, randomized, patient- and assessor-blinded, self-controlled clinical trial involving 491 adult patients with primary bilateral inguinal hernias. Conducted across 21 certified German hernia centers between August 2017 and February 2021, the trial employed a randomized allocation of mesh type to either the right or left side, ensuring each patient served as their own control.
All patients underwent standardized laparoendoscopic repair techniques—either transabdominal preperitoneal plasty (TAPP) or total extraperitoneal plasty (TEP). One side received a biological mesh implant, while the contralateral side received a synthetic mesh. The principal outcomes measured were pain intensity at 6 months, assessed by the visual analog scale (VAS), and hernia recurrence at 2 years. Secondary outcomes included rates of seroma, hematoma, surgical site infection, and patient satisfaction.
Key Findings
The trial enrolled predominantly male patients (93.1%), with a mean age of 58.5 years. Analysis revealed no significant difference in pain levels at rest at 6 months post-surgery between biological and synthetic mesh sides, with both groups reporting very low mean VAS scores (0.3 ± 0.9; P = .76).
However, significant disparities emerged regarding long-term hernia recurrence: biological meshes exhibited a markedly higher 2-year recurrence rate (11.2%, 53 recurrences) compared to synthetic meshes (2.5%, 12 recurrences), achieving high statistical significance (P < .001). This represents an approximately fourfold increased relative risk of recurrence with biological implants.
Secondary outcomes further highlighted safety concerns with biological meshes. Seroma formation was notably increased on the biological mesh side (33.4% vs 21.6%; P < .001), a complication that can prolong recovery and increase morbidity. No significant differences in hematoma or surgical site infection rates were reported.
Patient satisfaction did not differ appreciably between mesh types, consistent with the low reported pain levels.
Expert Commentary
The BIOLAP trial’s self-controlled design is a robust methodological strength, effectively controlling for interindividual variability, which is often a limitation in mesh comparison studies. Blinding of patients and assessors further reduces bias.
The lack of pain reduction despite the theoretical biocompatibility of biological meshes challenges assumptions about their benefit in minimizing chronic postoperative pain. The significantly higher recurrence rates observed suggest that biological meshes may not provide sufficient mechanical strength or durability to withstand the stresses in inguinal hernia repair, particularly in laparoendoscopic approaches.
Increased seroma formation with biological meshes could be related to the resorption and tissue remodeling processes inherent to these materials, leading to fluid collections. This raises concerns about postoperative complications and the need for additional interventions.
Limitations include the follow-up duration of 2 years; longer-term outcomes are still needed. Additionally, the study population was predominantly male and treated in highly specialized centers in Germany, which may affect generalizability to other populations or surgical settings.
Conclusion
The BIOLAP randomized clinical trial conclusively demonstrates that biological meshes do not confer a postoperative pain benefit over synthetic meshes in laparoendoscopic inguinal hernia repair. More importantly, they are associated with a significantly increased risk of hernia recurrence and seroma formation. These findings do not support the routine use of biological meshes for primary bilateral inguinal hernia repair using laparoendoscopic techniques.
For clinicians, synthetic mesh remains the gold standard for durable and safe hernia reinforcement in this context. Future research should focus on improving mesh materials to reduce pain and complications without compromising durability, as well as exploring patient-tailored approaches.
Reference
Seefeldt CS, Knievel J, Deeb M, Hoedt NT, Rudroff C, Essen R, Antoine D, Kaiser GM, Jacobi CA, Gross-Weege W, Gänsler W, Lammers BJ, Bonk C, Hildebrandt F, Carus T, Meyer M, Bebobru M, Krökel A, Dornbusch J, Schneider M, Cerasani N, Stechemesser B, Lefering R, Bulian DR, Ströhlein MA, Rieger A, Lange J, Meyer-Zillekens JS, Eisenberger CF, Heiss MM. Biological vs Synthetic Mesh in Laparoendoscopic Inguinal Hernia Repair: The BIOLAP Randomized Clinical Trial. JAMA Surg. 2025 Oct 8. doi: 10.1001/jamasurg.2025.4071. Epub ahead of print. PMID: 41060645. Trial registration: German Clinical Trials Register Identifier: DRKS00010178.