Highlights
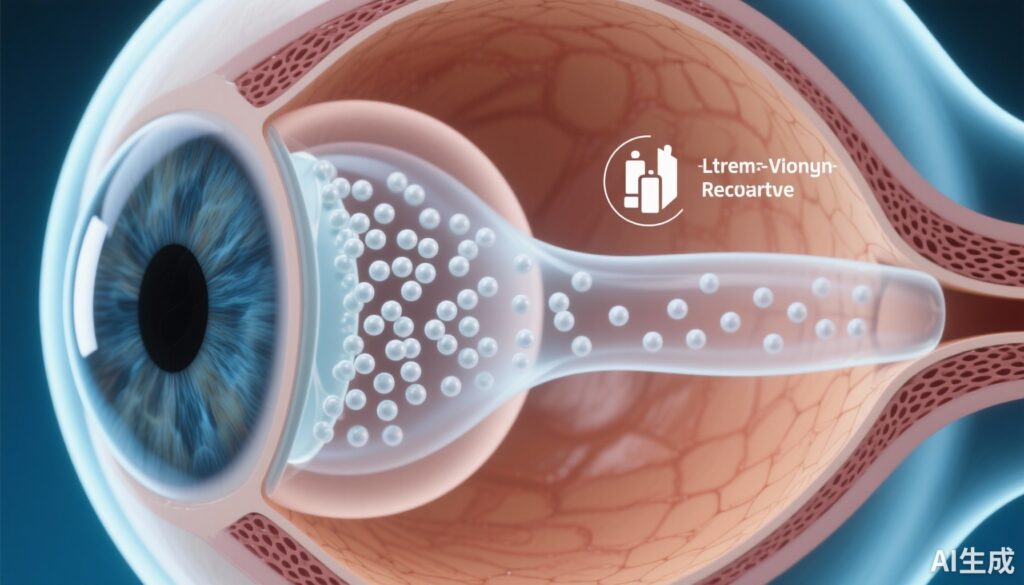
– A single intravitreal injection of a biodegradable aflibercept-loaded PLGA microsphere–thermo‑responsive hydrogel was visible in the vitreous and well tolerated in 23 rhesus macaques up to 24 months.
– No consistent adverse effects on intraocular pressure, corneal thickness, endothelial cells, axial length, refractive error, retinal thickness, retinal function (ERG), or retinal/choroidal vasculature (FA) were observed.
– Depot visualization persisted up to 9 months; histology in a subset (7 animals) showed preserved retinal architecture.
Background
Intravitreal anti–vascular endothelial growth factor (anti‑VEGF) injections such as aflibercept have transformed management of neovascular age‑related macular degeneration (AMD), diabetic macular edema, and other retinal vascular diseases. However, frequent injections are burdensome for patients and health systems and carry procedural risks. Extended‑duration intravitreal drug delivery systems (DDS) are a major unmet need to reduce visit frequency while maintaining efficacy and safety.
Biodegradable polymeric microspheres (commonly using poly(lactic‑co‑glycolic acid), PLGA) and in situ‑gelling hydrogels have been investigated as strategies to provide sustained intravitreal release. Non‑human primates (NHPs), particularly rhesus macaques, are a preferred preclinical model because of ocular anatomy and retinal similarities to humans, making biocompatibility and safety data in NHPs highly informative for translation.
Study design
This preclinical safety and biocompatibility study evaluated a novel biodegradable injectable microsphere‑hydrogel DDS loaded with aflibercept in healthy rhesus macaques. Key design elements included:
- Intervention: Aflibercept‑loaded PLGA microparticles prepared by a modified double emulsion technique, embedded in a thermo‑responsive poly(ethylene glycol)-co-(L‑lactic‑acid) diacrylate/N‑isopropylacrylamide hydrogel.
- Dose and administration: 50 µL intravitreal injection delivering 15 µg aflibercept into the right eye of each animal (n=23).
- Follow‑up: Monthly comprehensive ophthalmic assessments, including intraocular pressure (IOP), corneal pachymetry, specular microscopy, A‑scan biometry, streak retinoscopy, spectral‑domain optical coherence tomography (SD‑OCT), fluorescein angiography (FA), and electroretinography (ERG). Globes from a subset (7 animals) underwent histologic examination.
- Endpoints: Primary outcomes were local ocular tolerability and biocompatibility assessed clinically, structurally (OCT, FA), functionally (ERG), and histologically over follow‑up of up to 24 months.
Key findings
Depot persistence and ocular visibility
The intravitreal depot (aflibercept‑DDS) was visualized in the vitreous up to 9 months after injection. In 4 of 23 eyes the depot modestly impeded fundoscopy; in the remainder it did not interfere with clinical examination. The paper reports depot visualization but does not provide quantitative pharmacokinetic release curves in vitreous or retina.
Clinical safety and anterior segment outcomes
No consistent or clinically meaningful anterior segment adverse events were reported. Specifically:
- Intraocular pressure remained within normal limits at all measured timepoints.
- Central corneal thickness and endothelial cell density (specular microscopy) did not differ significantly from baseline.
- Axial globe length and refractive error (by A‑scan and retinoscopy) were unchanged.
Retinal structure and vascular integrity
SD‑OCT showed preservation of normal retinal architecture across animals and timepoints, with no significant change in total retinal thickness. Fluorescein angiography detected no retinal or choroidal vascular abnormalities attributable to the DDS; specifically, no leakage, nonperfusion, or neovascular events were reported.
Retinal function (ERG)
Full‑field ERG under scotopic and photopic conditions demonstrated no significant differences in implicit times or amplitudes for mixed rod‑cone or cone responses compared with baseline/control values, suggesting preserved global retinal function.
Histology
Histologic examination of globes from 7 animals showed preserved retinal cytoarchitecture and no consistent inflammatory infiltrates or toxic morphologic changes attributable to the DDS.
Duration of observation
Although the intravitreal depot was visibly present up to 9 months, the safety follow‑up extended to 24 months, during which animals remained free of consistent adverse structural or functional findings.
Interpreting the results
Collectively, these outcomes indicate that this PLGA microsphere‑in‑hydrogel delivery platform carrying aflibercept is well tolerated in the NHP eye after a single intravitreal injection at the tested dose. Preservation of retinal structure (OCT and histology), lack of angiographic abnormalities, and stable ERG responses are important preclinical signals supporting ocular biocompatibility.
Key caveats and nuances to interpretation include:
- The study was conducted in healthy eyes; responses in diseased (e.g., AMD, diabetic retinopathy) retinae, which may be more susceptible to inflammation or different local pharmacodynamics, were not assessed.
- Quantitative pharmacokinetic data (e.g., intraocular aflibercept concentrations over time) are not reported in the summary; visual persistence of the depot up to 9 months suggests sustained presence but does not directly define effective therapeutic levels.
- The single dose tested (15 µg) is substantially lower than typical clinical intravitreal aflibercept doses (e.g., 2 mg in humans); scaling and dose‑response will be critical for translation.
- Sample size for histology (7 animals) is modest; while no consistent adverse histologic findings were seen, rare events may be missed.
Expert commentary and context
Long‑acting intravitreal delivery is a major translational priority for retinal disease management. Current clinical strategies include refillable surgically implanted ports (for example, the ranibizumab port delivery system studied in human trials) and various sustained‑release biodegradable formulations under development. A biodegradable, injectable platform that avoids repeated intravitreal injections or surgical implants would offer practical advantages—minimally invasive administration, potential outpatient delivery, and elimination of implant removal or refilling procedures.
PLGA microspheres are among the most studied biodegradable carriers because of established biodegradability and regulatory precedence in other tissues and drug classes. Embedding microparticles within a thermo‑responsive hydrogel can limit particle dispersion, facilitate localization, and modulate release kinetics. The absence of ocular hypertension, endothelial toxicity, retinal structural damage, or functional deficits in NHPs in this study aligns with expectations for a well‑designed PLGA/hydrogel system, but human translation will require careful dose scaling and demonstration of therapeutic efficacy along with long‑term safety.
Limitations and unanswered questions
- Disease models and efficacy: Safety in healthy NHP eyes is necessary but insufficient. Future studies should test pharmacokinetics, functional efficacy, and safety in disease models (or early human trials) to determine whether therapeutic intraocular levels of aflibercept can be sustained for clinically meaningful durations.
- Dose scaling and formulation: The preclinical dose here (15 µg) is far below clinical human intravitreal doses; controlled dose‑escalation and optimization of release kinetics are needed to reach therapeutic concentrations safely in humans.
- Immunogenicity and biodegradation products: Long‑term immune responses, especially to polymer degradation products or possible aggregated protein from formulation processes, require further characterization including systemic antibody formation and local immune monitoring.
- Pharmacokinetics: Without vitreous/retinal drug concentration data over time, it is not possible to determine duration of therapeutic exposure from depot visualization alone.
- Interference with imaging or clinical care: Although the depot only modestly impeded fundoscopy in a minority of eyes, potential impacts on retinal monitoring (e.g., OCT image quality, laser procedures) should be evaluated in clinical contexts.
Translational implications and next steps
The favorable NHP safety profile supports progression to studies focused on pharmacokinetics, dose optimization, and efficacy. Recommended next steps include:
- Preclinical pharmacokinetic studies measuring intraocular drug concentrations over time to define release kinetics and correlate with depot visualization.
- Dose‑escalation safety studies and disease‑model experiments (e.g., laser‑induced CNV in NHPs or other relevant models) to test therapeutic effect and refine dosing.
- Assessment of immunogenicity and monitoring for anti‑drug antibodies following repeated exposures or sustained release.
- Early phase human clinical trials with careful safety and efficacy endpoints, imaging compatibility assessments, and patient‑centred outcomes such as injection frequency reduction and visual acuity stabilization.
Conclusion
This study demonstrates that a novel biodegradable PLGA microsphere embedded within a thermo‑responsive hydrogel and loaded with aflibercept was well tolerated in healthy rhesus macaque eyes following a single intravitreal injection. Structural, functional, and histologic assessments up to 24 months revealed no consistent adverse effects. These preclinical safety data are encouraging and support further pharmacokinetic, efficacy, and translational development toward a sustained intravitreal anti‑VEGF delivery strategy that could reduce treatment burden in retinal disease.
Funding and clinicaltrials.gov
The published article should be consulted for specific funding disclosures and conflicts of interest (Story BD et al., Drug Deliv. 2025). No clinicaltrials.gov identifier is provided in the preclinical report; subsequent human studies would require registration.
References
1. Story BD, Park S, Roszak K, Shim J, Motta M, Ferneding M, Rudeen KM, Blandino A, Ardon M, Le S, Teixeira LBC, Yiu G, Mieler WF, Thomasy SM, Kang‑Mieler JJ. Safety and biocompatibility of a novel biodegradable aflibercept‑drug delivery system in rhesus macaques. Drug Deliv. 2025 Dec;32(1):2460671. doi: 10.1080/10717544.2025.2460671. Epub 2025 Mar 4. PMID: 40038090; PMCID: PMC11884103.
2. Danhier F, Ansorena E, Silva JM, Coco R, Le Breton A, Préat V. PLGA‑based nanoparticles: an overview of biomedical applications. J Control Release. 2012 Jul 20;161(2):505–522. doi:10.1016/j.jconrel.2012.01.043.
3. Heier JS, Brown DM, Chong V, Korobelnik J‑F, Kaiser PK, Nguyen QD, et al. Intravitreal aflibercept (VEGF Trap‑Eye) in wet age‑related macular degeneration. Ophthalmology. 2012;119(12):2537–2548. (VIEW1 and VIEW2 pooled analyses).
AI thumbnail prompt
High‑detail medical illustration of a human eye in cross‑section showing an intravitreal depot composed of small biodegradable microspheres embedded in a translucent hydrogel within the vitreous cavity; include a label for ‘aflibercept’, a subtle timeline bar indicating ‘sustained release’, and a preserved macula/retina with intact layers visible on the illustration background. Clean clinical color palette, realistic anatomical textures, and a calm clinical tone.