Highlight
– A comparative effectiveness study assessed outcomes of acute surgical evacuation versus initial conservative treatment for acute subdural hematoma (ASDH) in trauma patients.
– Among 711 patients with ASDH, 21% underwent acute surgery, predominantly decompressive craniectomy, while 79% received conservative treatment.
– There was significant variability in surgical intervention rates between trauma centers with similar patient prognoses.
– No meaningful difference in 6-month functional outcomes was observed between centers favoring surgery versus conservative management, suggesting conservative treatment could be a viable option when clinical equipoise exists.
Study Background and Disease Burden
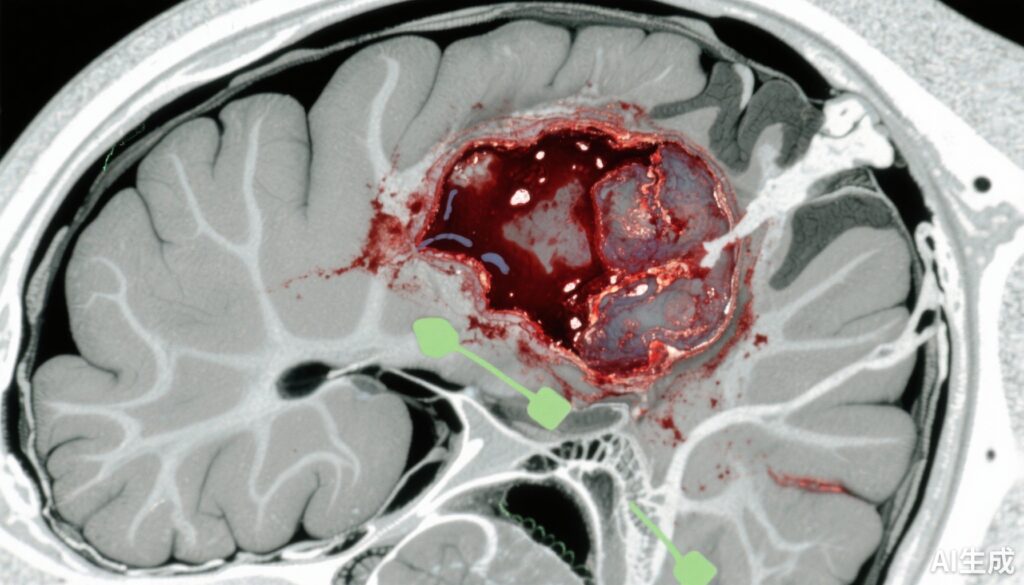
Traumatic brain injury (TBI) remains a major cause of morbidity and mortality worldwide, with acute subdural hematoma (ASDH) representing one of the most critical intracranial lesions. ASDH results from bleeding between the dura mater and the brain surface, often due to head trauma, leading to increased intracranial pressure and potential herniation. Traditional management involves emergent surgical evacuation to reduce mass effect and secondary brain injury. However, the heterogeneity of injury severity and patient factors has left uncertainty whether immediate surgery confers superior outcomes compared to conservative treatment in many cases. This uncertainty generates variability in clinical practice and highlights an unmet medical need to clarify optimal treatment strategies that balance risks and benefits in ASDH management.
Study Design
This comparative effectiveness study analyzed data from the prospective observational Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI) Study, which enrolled patients from February 1, 2014, to July 31, 2018. The setting comprised 18 Level 1 trauma centers across the United States. Inclusion criteria included patients with nonpenetrating TBI who presented to the emergency department and were admitted within 24 hours after injury with ASDH verified by acute head computed tomography (CT) scan.
Two treatment exposure groups were compared: acute surgical hematoma evacuation (predominantly decompressive craniectomy or craniotomy performed acutely) versus initial conservative treatment without immediate surgery. Centers were assessed based on their treatment preference profile, quantified by the case mix-adjusted likelihood of a patient undergoing acute surgery at that center.
The primary outcome measure was functional disability assessed at 6 months post-injury using the Glasgow Outcome Scale-Extended (GOS-E), analyzed using ordinal logistic regression adjusted for prespecified confounders. Variation in treatment preferences between centers was evaluated with a median odds ratio (MOR).
Statistical analyses were conducted from December 1, 2022, to December 20, 2024.
Key Findings
Out of 2697 enrolled patients, 711 (mean age 46.5 years, 76% male) met criteria for ASDH. Among these, 148 (21%) underwent acute cranial surgery, while 563 (79%) received initial conservative treatment.
Baseline differences highlighted a sicker surgical cohort: they had lower Glasgow Coma Scale (GCS) scores (mean 6.8 vs 11.4), a higher incidence of bilateral unreactive pupils (32% vs 9%), and more concurrent intracranial lesions (69% vs 53%) compared to the conservative treatment group. In the surgical cohort, 87% underwent decompressive craniectomy, and 11% underwent craniotomy. Among conservatively managed patients, 12% eventually required delayed surgery.
A remarkable discovery was the extensive variability in the proportion of patients receiving acute surgery across centers, ranging from 0% to 86%, with a median center-specific surgery rate of 17%. The MOR of 2.95 indicated a nearly threefold higher likelihood for similar patients to undergo surgery depending solely on the treating center’s preference.
Importantly, centers with a higher preference for acute surgical intervention did not demonstrate superior 6-month functional outcomes. The adjusted common odds ratio for improved outcome per 22% increase in acute surgery rate was 1.05 (95% CI, 0.88-1.26, P=0.06), indicating no statistically significant benefit of surgical over conservative initial treatment in this observational comparative effectiveness context.
Expert Commentary
This robust multicenter observational analysis offers critical insight into the complex decision-making landscape for ASDH management. The substantial inter-center variability with similar patient prognoses reflects the absence of a clear consensus and underscores reliance on institutional culture or surgeon preference rather than definitive evidence.
Notably, the lack of outcome advantage among centers favoring acute surgery amplifies the argument that conservative management remains a reasonable strategy for well-selected patients, especially those for whom neurosurgeons perceive clinical equipoise. Conservative management reduces exposure to surgical risks such as infection, hemorrhage, and anesthesia-related complications while allowing time for neurological stabilization.
However, the study’s observational design implies potential confounding by indication despite rigorous case mix adjustment. Patients undergoing surgery had more severe presentations, which might bias the results despite statistical efforts to control confounders. The delay in surgery for a subset of initially conservatively treated patients also suggests the importance of close monitoring with readiness to intervene if clinical deterioration occurs.
Current guidelines emphasize individualized decision-making integrating clinical, radiological, and physiological parameters. This study advances this framework by supporting initial conservative treatment as a viable option in selected ASDH cases, challenging the dogma of indiscriminate early surgery.
Future prospective randomized controlled trials are warranted to provide higher-level evidence and ideally delineate clear criteria for surgical versus conservative pathways, potentially incorporating advanced imaging and biomarker data.
Conclusions
In this large, multicenter comparative effectiveness study, patients with traumatic acute subdural hematomas were managed variably according to center-specific treatment preferences. Functional outcomes at 6 months did not differ between centers favoring acute surgical evacuation and those preferring initial conservative treatment after risk adjustment.
These findings suggest that conservative treatment should be considered when clinical equipoise exists, enabling tailored care that may avoid unnecessary surgical risks without compromising patient outcomes. Close monitoring to identify patients requiring delayed surgery remains paramount. This evidence supports a nuanced, patient-centered approach to ASDH management and highlights the need for randomized trials to refine practice guidelines and optimize outcomes.
References
1. Van Essen TA, Yue JK, Barber J, et al. Acute Surgery vs Conservative Treatment for Traumatic Acute Subdural Hematoma. JAMA Netw Open. 2025;8(10):e2535200. doi:10.1001/jamanetworkopen.2025.35200
2. Bullock MR, Chesnut R, Ghajar J, et al. Surgical Management of Acute Subdural Hematomas. Neurosurgery. 2006 May;58(3 Suppl):S2-11.
3. Maas AIR, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;7(8):728-741.
4. Stiver SI. Management of acute subdural hematoma. Neurosurg Focus. 2009;26(6):E7.
5. American Association of Neurological Surgeons; Congress of Neurological Surgeons. Guidelines for the Management of Severe Traumatic Brain Injury. https://www.braintrauma.org/coma/guidelines