Highlights
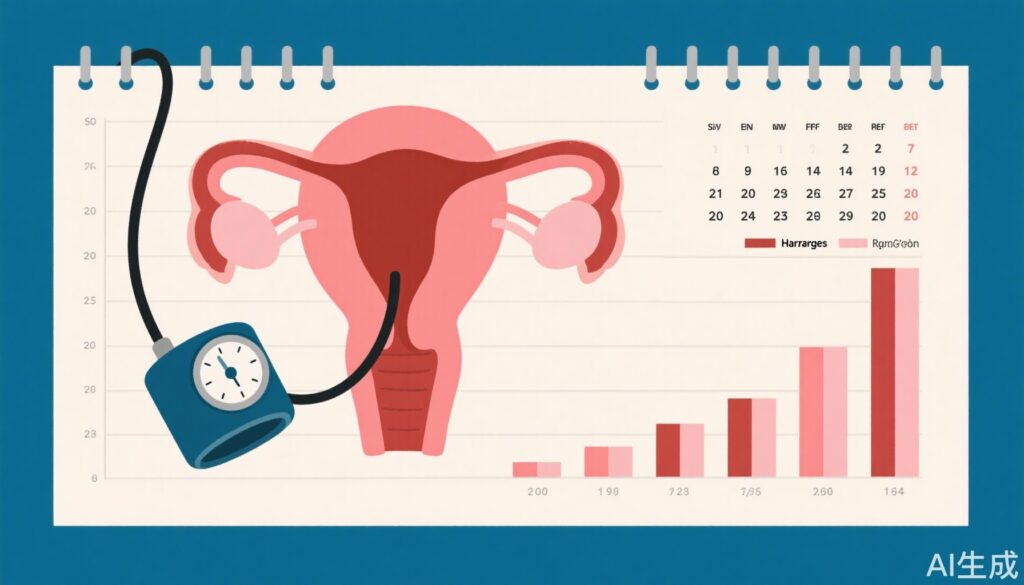
- Hysterectomy is linked to an 11% increased risk of incident hypertension in Korean women aged 40 to 59 years.
- The risk of hypertension was especially prominent in women with a hemoglobin increase of ≥2 g/dL post-hysterectomy.
- Adnexa-sparing hysterectomy was associated with a higher hypertension risk compared to nonhysterectomy controls, highlighting surgical approach relevance.
- This large-scale, long-term cohort with propensity score matching provides robust epidemiologic evidence to inform clinical decision-making.
Background
Hypertension remains a leading cardiovascular risk factor worldwide with significant morbidity and mortality. In women, various gynecological interventions—such as hysterectomy—have been hypothesized to impact cardiovascular health potentially through hormonal and vascular mechanisms. Hysterectomy is a common surgical treatment for benign gynecological conditions, but its systemic effects beyond reproductive health are not fully elucidated.
Prior studies examining the relationship between hysterectomy and hypertension have yielded conflicting results, partly due to limited sample sizes, heterogeneous populations, and differing study designs. Given the high prevalence of hysterectomy and hypertension in adult women, clarifying this association is clinically important for long-term management and risk stratification.
Key Content
Study Design and Population
This Korean nationwide cohort study retrospectively analyzed data from 802,916 women aged 40 to 59 years collected between 2002 and 2011. A total of 13,650 hysterectomy and nonhysterectomy matched pairs were created by 1:1 propensity score matching, adjusting for confounders such as age, socioeconomic status, comorbidities, and baseline hemoglobin levels.
Subjects were followed longitudinally until December 31, 2020, enabling a median follow-up exceeding 10 years. The primary endpoint was the incidence of hypertension identified through clinical and administrative health data.
Incidence and Risk Analysis
The incidence rates of hypertension were 22 and 20 per 1000 person-years in the hysterectomy and nonhysterectomy groups, respectively. After controlling for covariates, hysterectomy was associated with a statistically significant hazard ratio (HR) of 1.11 (95% CI, 1.05–1.17, P<.001), indicating a modest increase in hypertension risk.
Critically, the risk elevation was most notable in women who exhibited a post-procedural hemoglobin increase ≥2 g/dL, suggesting a possible biological link between hematologic changes and vascular tone or volume status influencing blood pressure regulation.
Subgroup Analysis: Impact of Adnexa Preservation
Women undergoing adnexa-sparing hysterectomy had a higher hypertension incidence (HR 1.15; 95% CI, 1.08–1.23; P<.001) compared to those who did not have hysterectomy. This finding suggests that preserving ovarian function while removing the uterus may not fully mitigate cardiovascular risks, and hormonal or structural vascular influences warrant further investigation.
Comparison With Existing Literature
Previous smaller studies and meta-analyses have produced mixed results regarding the hysterectomy-hypertension link. For example, some observational cohort studies showed no significant association, while others identified increased hypertension risks post-hysterectomy, especially when combined with oophorectomy.
This study’s strength lies in its large scale, propensity-matched design, and long follow-up, providing compelling evidence that supports a causal relationship, though the effect size remains moderate.
Potential Mechanisms
The biological plausibility of hysterectomy affecting hypertension risk may involve several pathways:
- Altered estrogen and progesterone signaling impacting vascular endothelial function and arterial stiffness.
- Changes in hematologic parameters influencing blood viscosity and systemic vascular resistance.
- Disruption of uterine or ovarian vascular structures potentially modulating systemic hemodynamics.
Further mechanistic studies are needed to elucidate these pathways.
Expert Commentary
This comprehensive nationwide cohort study offers important evidence linking hysterectomy to elevated hypertension incidence, informing clinicians to monitor blood pressure vigilantly after hysterectomy. However, the magnitude of increased risk is modest, and clinical decisions should balance the benefits of the surgical intervention against cardiovascular risk factors.
Guidelines for post-hysterectomy care may consider integrating cardiovascular risk assessments and personalized blood pressure control strategies. Moreover, the specific role of adnexa preservation necessitates further clinical trials to optimize surgical approach considering long-term cardiovascular outcomes.
Limitations include the observational study design, potential residual confounding despite propensity matching, and lack of detailed hormonal replacement therapy data. Nonetheless, the extended follow-up and large population base improve generalizability in East Asian populations.
Conclusion
In summary, hysterectomy in Korean women aged 40 to 59 years is associated with a modest but statistically significant increase in hypertension risk over a median 10-year follow-up. This risk is accentuated in women with increased post-surgical hemoglobin and those undergoing adnexa-sparing procedures.
Clinicians should consider cardiovascular monitoring as part of holistic post-hysterectomy management. Future research should focus on elucidating pathophysiological mechanisms and evaluating the impact of different surgical techniques and adjuvant therapies on cardiovascular risk.
References
- Yuk JS, Kim GS, Kim DG, Byun YS, Kim MH, Yoon SH, Han GH, Lee BK, Kim BG. Association of Hysterectomy With Hypertension Incidence in Korean Women: A Nationwide Cohort Study. Mayo Clin Proc. 2025 Aug 2:S0025-6196(25)00223-X. doi: 10.1016/j.mayocp.2025.04.015