Study Background and Disease Burden
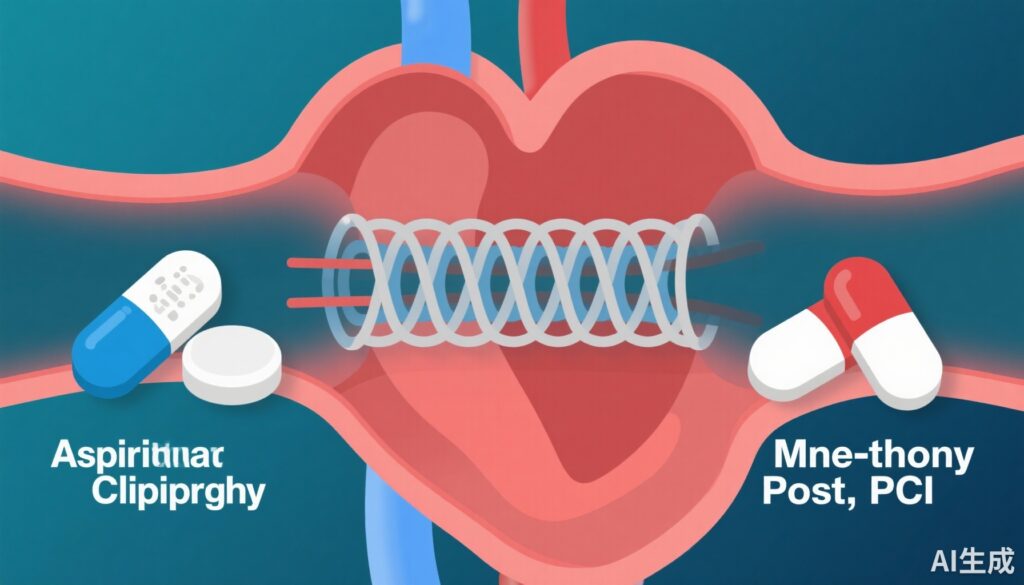
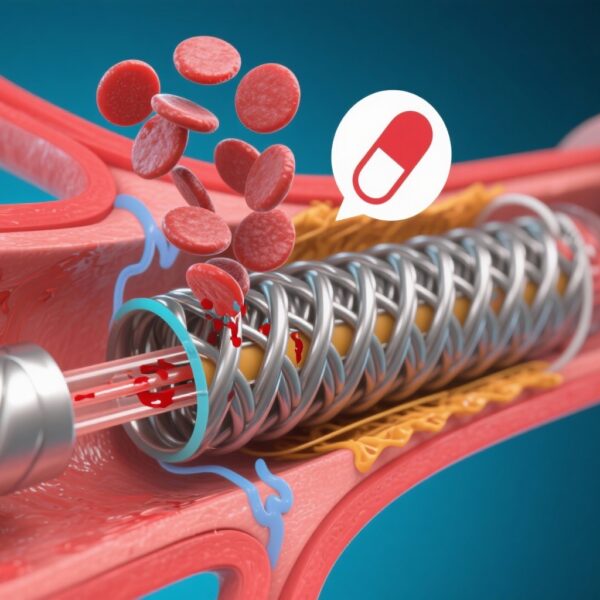
Percutaneous coronary intervention (PCI) with drug-eluting stents (DES) is a cornerstone treatment for coronary artery disease (CAD), especially in patients with acute coronary syndrome (ACS). Post-PCI, dual antiplatelet therapy (DAPT)—typically aspirin combined with a P2Y12 inhibitor—is recommended to reduce thrombotic complications such as stent thrombosis and recurrent ischemic events. However, prolonged DAPT increases bleeding risk, particularly in patients with high bleeding risk (HBR). Recent clinical practice has evolved towards shortening DAPT duration followed by monotherapy to balance ischemic protection and bleeding risk.
Until recently, no randomized controlled trial had directly compared aspirin monotherapy against P2Y12 inhibitor monotherapy after abbreviated DAPT following PCI. This knowledge gap is critical given the widespread use of aspirin historically, whereas P2Y12 inhibitors such as clopidogrel have emerged as alternative monotherapies with potentially different efficacy and safety profiles. The STOPDAPT-3 trial addresses this gap by evaluating the outcomes of aspirin versus clopidogrel monotherapy after short DAPT, focusing on cardiovascular and bleeding events over a one-year period.
Study Design
The STOPDAPT-3 trial enrolled 6002 patients who underwent PCI with DES, including those presenting with ACS or classified as having HBR. The study employed a randomized, open-label design with two arms:
– Aspirin group: One month of dual antiplatelet therapy with aspirin plus prasugrel, followed by aspirin monotherapy.
– Clopidogrel group: One month of prasugrel monotherapy, followed by clopidogrel monotherapy.
A secondary analysis involved a 30-day landmark approach, focusing on outcomes beyond the initial month when monotherapy was initiated. The co-primary endpoints included:
1. Cardiovascular endpoint, defined as a composite of cardiovascular death, myocardial infarction, definite stent thrombosis, or ischemic stroke.
2. Bleeding endpoint, defined as Bleeding Academic Research Consortium (BARC) type 3 or 5 bleeding.
Demographic and clinical characteristics were balanced between groups, with a median age of 73 years, 23.4% female patients, 74.6% presenting with ACS, and 54.1% categorized as HBR.
Key Findings
Of the 6002 randomized patients, 5833 (aspirin group: 2920; clopidogrel group: 2913) were included in the 30-day landmark analysis. Adherence to assigned monotherapy at one year was high and comparable between groups (87.5% aspirin, 87.2% clopidogrel).
The incidence of the cardiovascular endpoint beyond 30 days up to one year was equivalent between groups, with rates of 4.5 events per 100 person-years. The hazard ratio (HR) for aspirin vs. clopidogrel was 1.00 (95% confidence interval [CI]: 0.77–1.30; P=0.97), indicating no difference in ischemic risk.
Similarly, bleeding events (BARC 3 or 5) were comparable: 2.0 vs. 1.9 per 100 person-years, with an HR of 1.02 (95% CI: 0.69–1.52; P=0.92).
These findings suggest that aspirin monotherapy after short DAPT is neither superior nor inferior to clopidogrel monotherapy with respect to preventing cardiovascular events or major bleeding complications in this high-risk population.
Expert Commentary
The STOPDAPT-3 1-year follow-up provides critical evidence that aspirin and clopidogrel monotherapy post-short DAPT can be viewed as interchangeable concerning ischemic and bleeding endpoints. This mirrors an evolving paradigm questioning aspirin’s supremacy in antiplatelet monotherapy post-PCI, especially in the context of potent P2Y12 inhibitors.
Given the median patient age and high prevalence of ACS and HBR, the study population is representative of contemporary clinical practice, enhancing the generalizability of results. However, limitations include the open-label design and the fact that only Japanese centers participated, which may influence genetic and clinical response to antiplatelet agents.
Mechanistically, P2Y12 inhibitors like clopidogrel directly block platelet activation pathways distinct from aspirin’s cyclooxygenase inhibition. The similar outcomes may reflect adequate platelet inhibition by either strategy when applied following a short initial DAPT period.
This trial complements existing evidence from studies such as the GLOBAL LEADERS and TWILIGHT trials, which have explored de-escalation strategies but did not directly compare aspirin monotherapy to P2Y12 inhibitor monotherapy. The STOPDAPT-3 findings may encourage clinicians to tailor monotherapy choices based on patient tolerance, risk profiles, and drug availability rather than default aspirin use.
Conclusion
The 1-year follow-up analysis of the STOPDAPT-3 trial demonstrates that aspirin monotherapy and clopidogrel monotherapy after short-term DAPT have comparable cardiovascular and bleeding outcomes in patients undergoing PCI with drug-eluting stents. This evidence supports the clinical flexibility in selecting antiplatelet monotherapy post-PCI, potentially improving patient-centered care by enabling individualized antithrombotic strategies, especially in populations at high bleeding risk.
Future research should focus on broader populations, longer-term outcomes, and stratification by genetic factors affecting clopidogrel metabolism to further optimize post-PCI antiplatelet therapy.
References
1. Watanabe H, Natsuaki M, Morimoto T, et al. Aspirin vs. clopidogrel monotherapy after percutaneous coronary intervention: 1-year follow-up of the STOPDAPT-3 trial. Eur Heart J. 2024 Dec 16;45(47):5042-5054. doi: 10.1093/eurheartj/ehae617.
2. Mehran R, Baber U, Sharma SK, et al. Ticagrelor with or without Aspirin in High-Risk Patients after PCI. N Engl J Med. 2019;381(21):2032-2042.
3. Valgimigli M, Bueno H, Byrne RA, et al. ESC focused update on dual antiplatelet therapy in coronary artery disease. Eur Heart J. 2018;39(3):213-260.