Introduction: The Conundrum of Antithrombotic Management Post-PCI
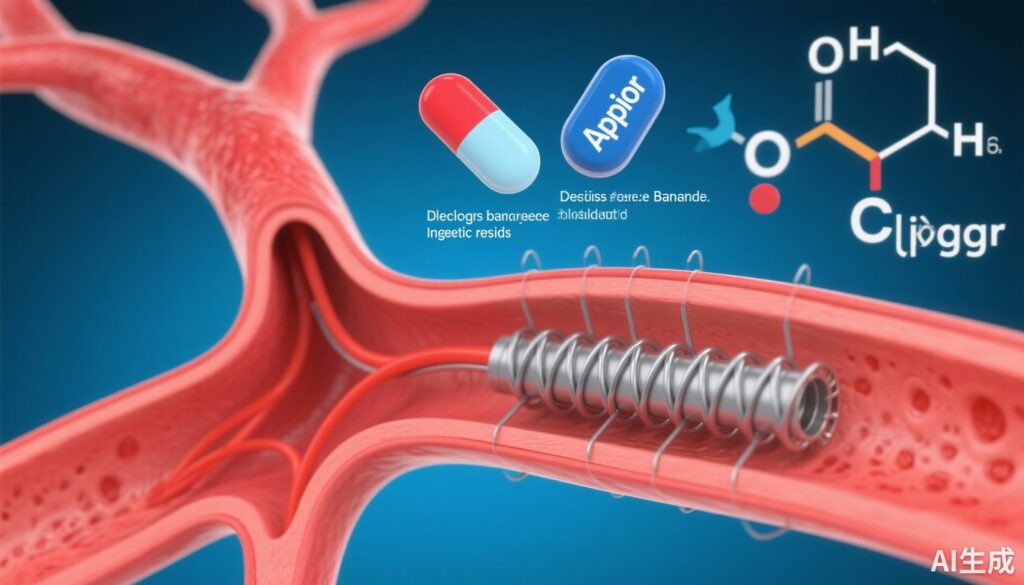
The management of patients undergoing percutaneous coronary intervention (PCI) who also require long-term oral anticoagulation (OAC)—primarily due to atrial fibrillation or prosthetic heart valves—remains one of the most complex challenges in clinical cardiology. This population exists at the intersection of high ischemic risk and high bleeding risk. Historically, the standard of care involved triple therapy (aspirin, a P2Y12 inhibitor, and OAC). However, the significant bleeding burden associated with triple therapy led to a shift toward double therapy, typically consisting of OAC and a P2Y12 inhibitor, usually clopidogrel.
While several landmark trials like PIONEER AF-PCI, REDUAL-PCI, and AUGUSTUS have established the safety of dropping aspirin early in favor of double therapy, a specific question remained under-investigated: once the initial high-risk period (the first month) has passed, does it matter which antiplatelet agent is used alongside OAC? Specifically, how does aspirin monotherapy compare to clopidogrel monotherapy in the maintenance phase (1 to 12 months) post-PCI, particularly for those already on OAC? The STOPDAPT-3 subgroup analysis, recently published in Circulation: Cardiovascular Interventions, provides much-needed clarity on this clinical uncertainty.
Study Design and Methodology: A Landmark Perspective
The STOPDAPT-3 trial (Short and Optimal Duration of Dual Antiplatelet Therapy-3) was originally designed to evaluate an aspirin-free strategy. It compared a 1-month dual antiplatelet therapy (DAPT) regimen followed by aspirin monotherapy (the aspirin group) with a 1-month prasugrel monotherapy followed by clopidogrel monotherapy (the clopidogrel group).
This specific subgroup analysis utilized a 30-day landmark approach. This means the researchers focused exclusively on events occurring after the first 30 days post-procedure up to the one-year mark. The study population consisted of 5,809 patients who were alive and free of major events at the 30-day mark. Within this cohort, 788 patients (13.6%) were receiving OAC at the time of discharge.
The investigators stratified the patients into two main cohorts: those with OAC and those without. They then compared the outcomes of the aspirin group versus the clopidogrel group within these strata. The primary endpoints were twofold:
1. Cardiovascular endpoints: A composite of cardiovascular death, myocardial infarction (MI), definite stent thrombosis, or ischemic stroke.
2. Bleeding endpoints: Defined as Bleeding Academic Research Consortium (BARC) type 3 or 5 (major bleeding).
Key Findings: Parity in Efficacy and Safety
The results of the 30-day landmark analysis suggest a remarkable degree of parity between aspirin and clopidogrel in the maintenance phase of post-PCI care, regardless of the patient’s anticoagulation status.
Cardiovascular Outcomes
Among the 788 patients on OAC, the incidence of cardiovascular events beyond 30 days was 3.7% in the aspirin group and 3.9% in the clopidogrel group. The resulting hazard ratio (HR) was 0.92 (95% CI, 0.44–1.93). In patients not receiving OAC, the rates were similarly matched: 3.7% for aspirin versus 3.6% for clopidogrel (HR, 1.03; 95% CI, 0.77–1.38). Critically, the P-interaction value was 0.78, indicating that the effect of the antiplatelet choice did not significantly differ based on whether the patient was taking an oral anticoagulant.
Bleeding Outcomes
Safety results followed a similar trend. In the OAC cohort, major bleeding (BARC 3 or 5) occurred in 3.5% of the aspirin group compared to 4.2% of the clopidogrel group (HR, 0.82; 95% CI, 0.39–1.73). In the no-OAC cohort, bleeding rates were 1.5% and 1.4%, respectively (HR, 1.07; 95% CI, 0.66–1.72). The P-interaction for bleeding was 0.57, again confirming that OAC status did not modify the relative safety profiles of these two antiplatelet agents.
Expert Commentary: Interpreting the Data in Clinical Context
These findings are significant because they offer clinicians flexibility. For many years, clopidogrel has been the preferred P2Y12 inhibitor for use alongside OAC due to its lower bleeding profile compared to more potent agents like prasugrel or ticagrelor. However, the choice between aspirin and clopidogrel as the single antiplatelet component of a double-therapy regimen after the first month has often been debated.
The STOPDAPT-3 data suggest that beyond the first month, the specific choice of the single antiplatelet agent—aspirin or clopidogrel—may be less critical than previously thought. This is particularly relevant for patients who might have a specific intolerance to one agent, such as aspirin-induced gastrointestinal distress or clopidogrel resistance (due to CYP2C19 polymorphisms).
However, some limitations must be acknowledged. First, this is a subgroup analysis of a larger trial, and the OAC cohort (N=788) is relatively small compared to the non-OAC cohort. This may limit the statistical power to detect very small differences in rare events like stent thrombosis. Second, the “clopidogrel group” in this trial actually received prasugrel for the first 30 days, which is an unconventional approach in many health systems for patients also requiring OAC. Most current guidelines (such as the ESC and AHA/ACC guidelines) still lean toward clopidogrel as the default P2Y12 inhibitor in AF-PCI patients due to the robust evidence base from trials like AUGUSTUS.
From a mechanistic perspective, the lack of difference between aspirin and clopidogrel in the presence of OAC suggests that the OAC itself provides the bulk of the protection against thromboembolic events (like stroke), while the single antiplatelet agent provides sufficient protection against stent-related complications, with neither agent having a distinct advantage in the 1-to-12-month window.
Conclusion: Clinical Implications for the Maintenance Phase
The STOPDAPT-3 subgroup analysis provides reassuring evidence that for patients who have successfully navigated the first 30 days after PCI without a major event, both aspirin and clopidogrel are viable options for continued therapy up to one year. This equivalence holds true whether or not the patient requires concomitant oral anticoagulation.
For the practicing clinician, this means that if a patient on OAC develops a side effect to clopidogrel after the first month post-PCI, switching to aspirin monotherapy (plus OAC) is likely safe from both an ischemic and a bleeding standpoint. Conversely, for patients already on clopidogrel monotherapy (plus OAC), there is no compelling reason to switch to aspirin. This study reinforces the trend toward personalized antithrombotic therapy, where the choice of agent can be tailored to patient tolerance, cost, and genomic profile without compromising clinical outcomes.
Funding and Registration
This research was part of the STOPDAPT-3 trial. The trial is registered at ClinicalTrials.gov with the unique identifier NCT04609111.
References
1. Natsuaki M, Watanabe H, Morimoto T, et al. Aspirin Versus Clopidogrel Beyond 1 Month After PCI in Patients With Oral Anticoagulation. Circ Cardiovasc Interv. 2025;18(11):e015495.
2. Watanabe H, Morimoto T, Natsuaki M, et al. Comparison of An Aspirin-Free Strategy With Usual Dual Antiplatelet Therapy After Stenting for Coronary Artery Disease (STOPDAPT-3). Circulation. 2023;148.
3. Cannon CP, Bhatt DL, Oldgren J, et al. Dual Antithrombotic Therapy with Dabigatran after PCI in Atrial Fibrillation. N Engl J Med. 2017;377(15):1413-1424.
4. Lopes RD, Heizer G, Aronson R, et al. Antithrombotic Therapy after Percutaneous Coronary Intervention in Atrial Fibrillation. N Engl J Med. 2019;380(16):1509-1524.