Introduction
Chronic low back pain (CLBP) represents a major public health concern, particularly among older adults where its prevalence exceeds one-third of the population aged 65 years and older.1,3 This condition contributes significantly to pain-related disability worldwide and leads to high economic costs, with expenditures surpassing $134 billion annually in the United States alone.5 Conventional treatments, primarily pharmacologic and invasive modalities, have had limited long-term impact on improving functional outcomes in this demographic.6-13 The risk of adverse events related to polypharmacy in older adults further underscores the need for low-risk, nonpharmacologic management strategies.16-20
Acupuncture has demonstrated efficacy for CLBP and is endorsed as a first-line nonpharmacological treatment by guidelines such as those from the American College of Physicians.24,25 Moreover, acupuncture is associated with improvements in sleep quality and emotional well-being — common concerns in older populations with CLBP.28-30 However, there has been a lack of large-scale randomized clinical trials specifically targeting older adults, and optimal dosing strategies remain uncertain.
The Centers for Medicare & Medicaid Services’ inquiry into acupuncture coverage for Medicare beneficiaries with CLBP motivated the present multisite pragmatic randomized clinical trial to evaluate the effectiveness of standard acupuncture (SA) and enhanced acupuncture (EA) relative to usual medical care (UMC) alone in adults aged 65 years or older.
Study Design and Methods
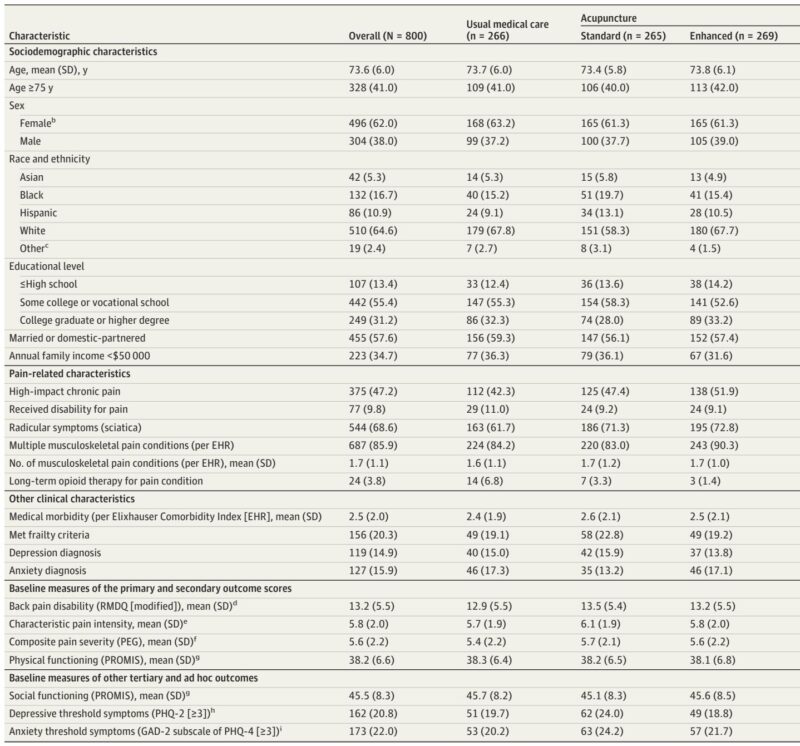
This 3-arm, parallel-group randomized clinical trial (BackInAction) was conducted across four US health care systems representing diverse geographic regions and delivery models: Kaiser Permanente Washington, Kaiser Permanente Northern California, Sutter Health, and The Institute for Family Health in New York City.31 Enrollment occurred between August 12, 2021, and October 27, 2022, with follow-up completed by November 7, 2023. Eligible participants were aged 65 or older, experiencing nonspecific CLBP for at least 3 months, with a minimum pain-related interference score of 3 on the PEG scale.35 Exclusions included serious spinal pathology, recent spine surgery, cognitive impairment, recent acupuncture treatment, or inability to attend sessions.
Randomization was stratified by site, age category, and sex, with participants assigned 1:1:1 to UMC, SA, or EA using concealed allocation through REDCap software. Blinding of participants to the receipt of maintenance acupuncture in the EA group was maintained until approximately 10 weeks post-randomization.
Interventions included SA consisting of 8-15 acupuncture sessions over 12 weeks plus UMC, and EA comprising the SA regimen plus 4-6 additional maintenance sessions during the subsequent 12 weeks. Acupuncture was delivered by over 50 licensed, community-based acupuncturists adhering to needle-only protocols aligned with Medicare coverage provisions.37,38 Participants in the UMC group were requested to avoid acupuncture during the study.
Outcomes
The primary outcome was the change in CLBP-related disability from baseline to six months, measured by the Roland-Morris Disability Questionnaire (RMDQ).41 Secondary outcomes comprised pain intensity (via PEG scale), rates of clinically meaningful improvement (≥30% reduction), Patient Global Impression of Change (PGIC), and measures of physical and social functioning (PROMIS), depression (PHQ-2), and anxiety (GAD-2).
Adverse events were monitored via reports from acupuncturists, participant follow-up, and medical record review, with serious events adjudicated for relatedness. Sample size calculations ensured 90% power to detect a 2-point mean RMDQ difference between groups at six months, accounting for a 20% missing data rate.
Statistical analyses employed generalized estimating equations to model outcomes at 3, 6, and 12 months, adjusting for covariates and accounting for missing data through imputation and inverse probability weighting.
Key Findings
Of 1706 individuals screened, 800 participants (mean age 73.6 years; 62.0% female) were randomized: 266 to UMC, 265 to SA, and 269 to EA. Adherence was high, with over 80% of participants completing the minimum therapeutic acupuncture dose.
At 6 months, both SA and EA groups demonstrated statistically significant and clinically meaningful reductions in RMDQ scores compared to UMC (SA vs UMC adjusted mean difference [AMD]: −1.0; 95% CI, −1.9 to −0.1; EA vs UMC AMD: −1.5; 95% CI, −2.5 to −0.6), with effect sizes approximating small-to-moderate magnitude (standardized mean differences −0.21 and −0.32, respectively). No significant differences in RMDQ changes were observed between SA and EA. These benefits persisted through 12 months.
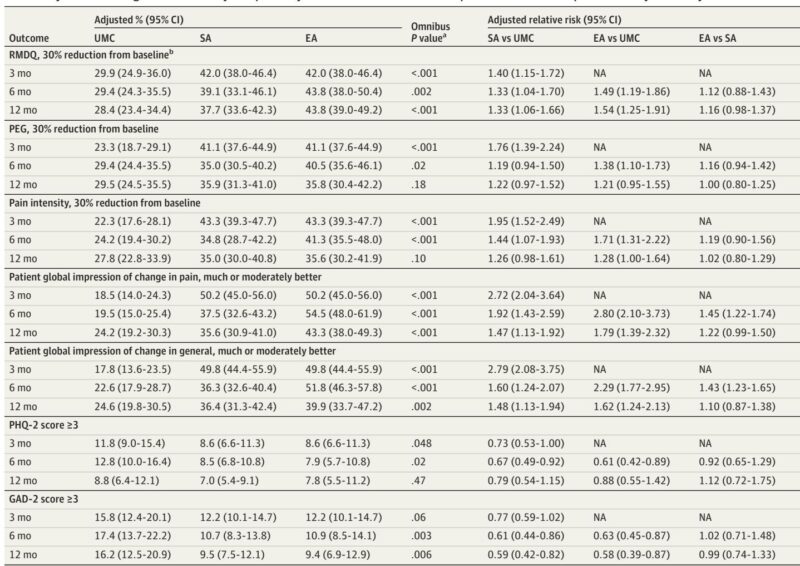
Pain intensity (PEG scale) also favored acupuncture, with EA exhibiting superior reductions versus SA at 6 months (AMD −0.5; 95% CI, −0.9 to −0.1). The proportion of participants achieving clinically meaningful improvements (≥30%) in RMDQ at 6 months was greater for SA (39.1%; relative risk [RR], 1.33; 95% CI, 1.04-1.70) and EA (43.8%; RR, 1.49; 95% CI, 1.19-1.86) compared with UMC (29.4%), with sustained advantages at one year.
Acupuncture groups also reported significant reductions in anxiety symptoms compared to UMC at 6 and 12 months. Other secondary outcomes, including physical and social functioning and depression, did not show consistent between-group differences.
Safety profiles were favorable, with serious adverse events rare and unrelated to acupuncture (less than 1% possibly related). Minor adverse events were infrequent and mainly consisted of local needling discomfort.
Expert Commentary
This pragmatic trial provides robust evidence supporting acupuncture needling as an effective and safe intervention for older adults with CLBP, a population often underrepresented in clinical research. The observed functional improvements align with or surpass outcomes reported in previous acupuncture studies targeting general adult populations,21-23,55 and offer advantages relative to pharmacologic treatments, which carry higher risks in the elderly.16-20
The absence of significant differences between standard and enhanced acupuncture regimens suggests that extending acupuncture with maintenance sessions may not yield additional functional benefits, although marked improvements in pain intensity with maintenance therapy warrant further exploration.
Limitations include the pragmatic design’s lack of sham control, precluding isolation of specific acupuncture effects versus nonspecific or placebo contributions. Notwithstanding, the comparison with usual care provides real-world relevance to clinical decision-making. The inability to fully assess medication usage changes and possible missing data bias constitute additional caveats.
Notably, expansion of Medicare coverage to include acupuncture without supervisory restrictions on licensed acupuncturists could enhance access for older patients, addressing current systemic barriers.37,64
Conclusion
In this large, multisite randomized clinical trial, acupuncture demonstrated clinically meaningful improvements in CLBP-related disability and pain among older adults relative to usual medical care, with sustained effects at 12 months and a low-risk profile. These findings endorse acupuncture needling as a viable, safe, and effective nonpharmacologic treatment option for managing chronic low back pain in the aging population.
Visual Abstract Image Prompt
“Illustration of a senior patient receiving acupuncture treatment on lower back, showing needle placements, with graphical overlay depicting improvement in disability scores and pain reduction over time, set against a backdrop of healthcare facilities in diverse geographic locations.”
Reference
DeBar LL, Wellman RD, Justice M, Avins AL, Beyrouty M, Eng CM, Herman PM, Nielsen A, Pressman A, Stone KL, Teets RY, Cook AJ. Acupuncture for Chronic Low Back Pain in Older Adults: A Randomized Clinical Trial. JAMA Netw Open. 2025 Sep 2;8(9):e2531348. doi: 10.1001/jamanetworkopen.2025.31348 IF: 9.7 Q1 . PMID: 40938602 IF: 9.7 Q1 ; PMCID: PMC12432643 IF: 9.7 Q1 .