Highlight
– AAV‑OTOF (Anc80L65 capsid) administered to 10 individuals with autosomal recessive deafness 9 (DFNB9) was well tolerated over 6–12 months and produced large, rapid improvements in auditory thresholds.
– Mean pure‑tone average (PTA) improved from 106 ± 9 dB to 52 ± 30 dB; click and tone‑burst ABR strongly predicted behavioral PTA after 4 months (R2 = 0.68 and 0.73).
– The therapeutic effect occurred largely within 1 month and showed an age‑dependent response with best outcomes in children aged 5–8 years; longer follow‑up is needed to confirm durability and late safety.
Background
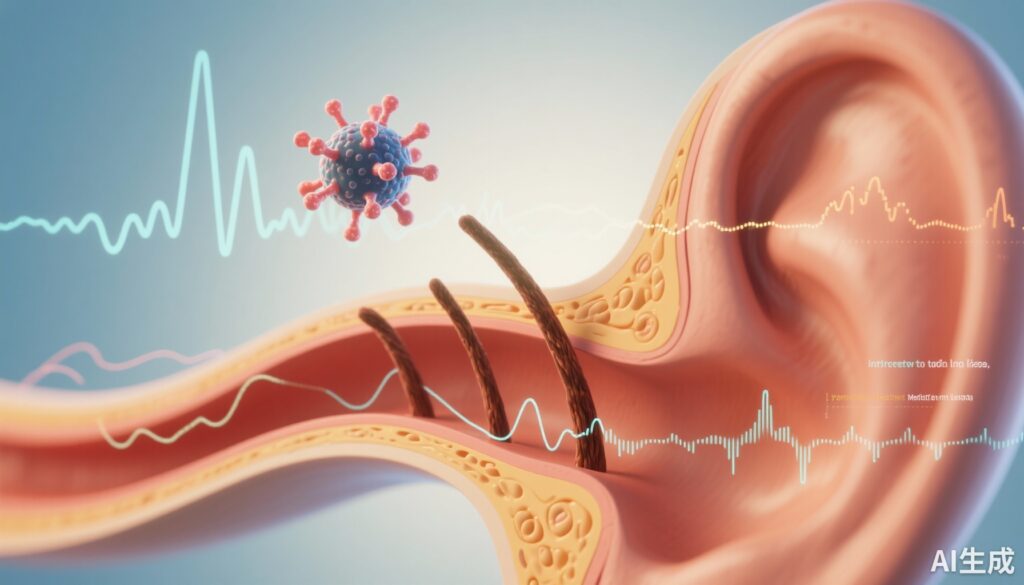
Hereditary congenital sensorineural hearing loss is a common sensory disorder with substantial functional and psychosocial impact. Mutations in OTOF, encoding otoferlin, cause autosomal recessive deafness 9 (DFNB9), typically characterized by severe‑to‑profound congenital auditory neuropathy owing to defective synaptic vesicle exocytosis at inner hair cell ribbon synapses. For many patients, hearing aids or cochlear implants are the mainstays of management; gene replacement to restore otoferlin function has been a longstanding therapeutic goal supported by preclinical models.
Study design
Qi et al. report an open‑label, single‑arm, multi‑site Phase 1/2 clinical trial of an adeno‑associated virus (AAV) vector encoding full‑length OTOF delivered using the synthetic Anc80L65 capsid (ClinicalTrials.gov NCT05901480). Ten genetically confirmed DFNB9 participants aged 1.5 to 23.9 years were treated at five sites in China; one participant received two injections. The primary endpoints were safety and tolerability out to 5 years; secondary endpoints assessed objective and behavioral auditory function, including pure‑tone average (PTA), click auditory brainstem response (ABR), tone‑burst ABR, and auditory steady‑state response (ASSR). Reported follow‑up ranged 6–12 months for the cohort described in this initial publication.
Key findings
Population and dosing
Ten participants with biallelic pathogenic OTOF variants received AAV‑OTOF. Ages at treatment spanned toddlerhood through young adulthood (1.5–23.9 years). Details of vector dose and surgical delivery approach (round window or cochleostomy, bilateral vs unilateral treatment strategy, and use of perioperative steroids) are described in the primary manuscript.
Safety and tolerability
The intervention was generally well tolerated over the 6–12‑month observation window. Investigators recorded 162 adverse events (AEs), all grade I or II in severity. The most frequent AE was decreased neutrophil percentage (16 of 162 events). No grade III–V events, vector‑related serious adverse events, or unexpected safety signals were reported during this early follow‑up. The authors emphasize ongoing monitoring for potential delayed immune, inflammatory, or ototoxic effects given the lifelong implications of in‑situ gene expression.
Efficacy — auditory thresholds and objective measures
All ten participants completed at least 6 months of follow‑up and showed marked improvement in hearing thresholds. Mean PTA improved from 106 ± 9 dB at baseline to 52 ± 30 dB after treatment. Objective electrophysiologic measures likewise improved: click ABR thresholds improved from 101 ± 1 dB to 48 ± 26 dB, tone‑burst ABR thresholds from 91 ± 4 dB to 57 ± 19 dB, and ASSR from 80 ± 14 dB to 64 ± 21 dB. These shifts represent clinically meaningful changes for most participants, converting many from the range of profound hearing loss to severe‑moderate loss on average.
Timecourse of benefit
Post hoc analyses indicated a rapid onset of effect: most of the hearing gains were achieved within the first month after treatment. Subsequent incremental improvements occurred but the bulk of threshold change was early, consistent with restoration of synaptic function once otoferlin expression was established.
Predictors of behavioral outcome
On an individual level, click and tone‑burst ABR thresholds correlated well with behavioral PTA after 4 months (R2 = 0.68 and 0.73, respectively), suggesting these objective electrophysiologic measures can reliably predict functional hearing once the therapeutic effect stabilizes. ASSR did not predict behavioral PTA (R2 = 0.17) in these analyses.
Age dependence
An age‑dependent therapeutic response was observed. The greatest and most consistent improvements were seen in children aged 5–8 years, suggesting a critical window in which inner ear circuits retain sufficient plasticity or neuronal integrity to benefit maximally from otoferlin replacement. Younger toddlers and older adolescents/young adults showed more variable responses. These findings are biologically plausible given developmental auditory pathway maturation and the time‑dependent degeneration of synaptic structures in congenital auditory synaptopathies.
Safety considerations and longer‑term uncertainties
Short‑term safety in this cohort was encouraging with no high‑grade AEs attributed to the vector or surgical procedure. However, important safety domains remain to be defined with longer follow‑up and larger cohorts: sustained immune responses to AAV capsids or transgene, off‑target transduction effects, inner ear inflammation or fibrosis, progression of cochlear pathology despite restored otoferlin, and any systemic sequelae. The observed transient neutrophil percentage changes merit monitoring but were not associated with clinical infections in the reported interval.
Expert commentary and contextualization
This report constitutes a major early milestone for human gene therapy for synaptic forms of congenital deafness. The magnitude and rapidity of threshold improvement in multiple objective modalities support biological plausibility: OTOF replacement in inner hair cells restores the calcium‑triggered exocytotic machinery required for faithful auditory signaling. The use of Anc80L65 — a capsid engineered for efficient inner ear transduction — aligns with preclinical data demonstrating robust hair cell targeting and functional rescue in Otof knockout models.
Clinically, the age effect has immediate implications for patient selection and counseling. The 5–8 year window of optimal response suggests prioritizing genetically confirmed DFNB9 patients in that age range for early access programs or trials, while recognizing that some benefit beyond this range is possible. These findings also raise practical questions about the interplay between AAV‑mediated gene restoration and cochlear implantation: whether gene therapy could reduce the need for implants in some patients or serve as an adjunct to optimize residual hearing remains to be defined.
Limitations
Key limitations of the current report include the single‑arm, open‑label design and small sample size, which preclude definitive efficacy estimates and increase susceptibility to selection bias. The relatively short follow‑up (6–12 months) does not address durability of benefit or late adverse events. Heterogeneity in age and possibly in dose or surgical approach complicate extrapolation to broader populations. Finally, the post hoc nature of predictor and subgroup analyses should be viewed as hypothesis‑generating; prospective validation is needed.
Clinical and research implications
These early results support continued development of AAV‑OTOF gene therapy and suggest several priorities: confirmatory studies with larger cohorts and longer follow‑up, randomized or controlled designs where feasible, systematic investigation of optimal dosing and delivery routes (including bilateral treatment), and mechanistic biomarker programs combining electrophysiology, imaging, and molecular assays to predict responders. From a clinical perspective, routine genetic testing for OTOF mutations in congenital/prelingual auditory neuropathy should be emphasized to identify treatment candidates early.
Conclusion
The single‑arm trial of AAV‑OTOF (Anc80L65) in 10 DFNB9 patients demonstrates promising early safety and clinically meaningful, rapid hearing improvements, with maximal effects observed in children aged 5–8 years. While encouraging, these preliminary data require confirmation in larger, longer‑duration studies to define durability, late safety, optimal patient selection, and integration with existing auditory rehabilitation strategies.
Funding and clinicaltrials.gov
Primary funding sources and trial sponsorship are reported in the original publication. The trial is registered at ClinicalTrials.gov: NCT05901480. Readers should consult the full article for detailed disclosures and site‑level information.
Reference
Qi J, Zhang L, Lu L, Tan F, Cheng C, Lu Y, Dong W, Zhou Y, Fu X, Jiang L, Tan C, Zhang S, Sun S, Song H, Duan M, Zha D, Sun Y, Gao X, Xu L, Zeng FG, Chai R. AAV gene therapy for autosomal recessive deafness 9: a single-arm trial. Nat Med. 2025 Sep;31(9):2917-2926. doi: 10.1038/s41591-025-03773-w. Epub 2025 Jul 2. PMID: 40603731.