Introduction: Beyond the Traditional Five Senses
Humans are commonly taught that we possess five fundamental senses: sight, hearing, smell, taste, and touch. Yet, scientists have long pondered whether an elusive “sixth sense” might exist, helping us navigate the world in ways not yet fully understood. Among the contenders is the ability to sense Earth’s magnetic fields, sometimes called “magnetoreception,” observed in other species but debated in humans. Another fascinating candidate centers on our gut—an organ long overlooked for its sensory capabilities.
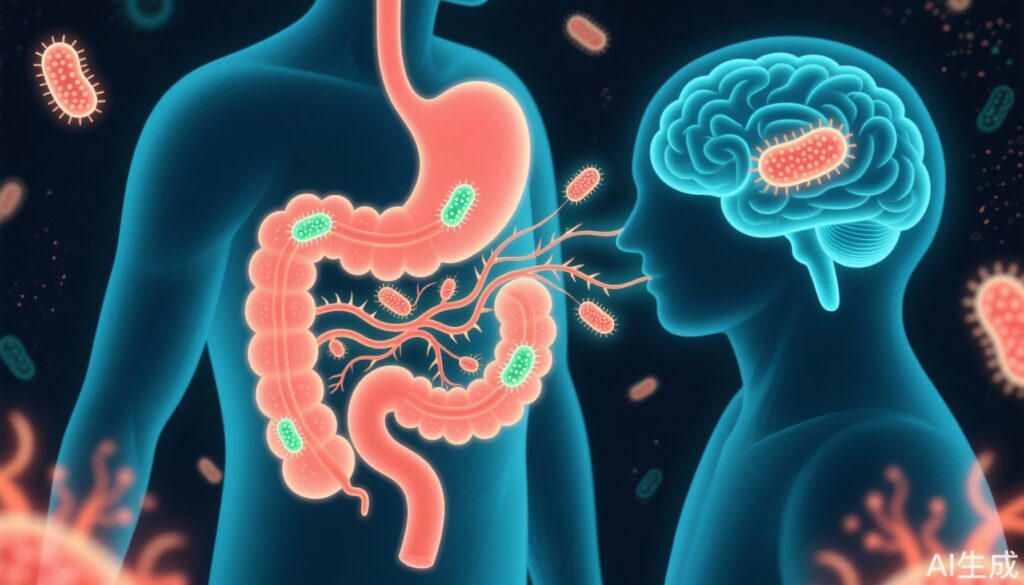
The human gut houses a complex ecosystem composed of trillions of microbes, forming a dynamic community that profoundly affects our physiology. Although we rarely consciously perceive these microorganisms, emerging evidence reveals the gut communicates continuously with the brain through the gut-brain axis. This communication influences a range of functions, notably appetite and feeding behavior.
Recent advances published in Nature have introduced a new concept termed “neurobiotic sense”—a sensory system within the gut epithelium that monitors specific microbial signals and modulates our eating habits accordingly. This discovery represents a paradigm shift in how we understand human sensory perception and metabolic regulation.
Understanding the Gut Microbiome and Its Influence
The human gastrointestinal tract is colonized by an astonishingly vast microbial population, consisting of bacteria, viruses, fungi, and archaea. These microorganisms constitute a mutually beneficial relationship: while microbes gain a nutrient-rich habitat, humans receive vital assistance in digestion, vitamin production, immune system training, and pathogen defense.
However, despite this mutualism, the gut environment is highly dynamic—microbial populations fluctuate in response to diet, stress, medications, and disease. How the host detects and responds in real-time to these shifts has remained an unanswered question until now.
The Discovery of Neurobiotic Sense
A groundbreaking study by a Duke University research team, recently published in Nature, sheds light on this mystery. The researchers identified specialized cells known as neuropod (or “nerve-foot”) cells embedded within the colonic epithelium. Although comprising a small fraction of epithelial cells, these neuropod cells exhibit remarkable sensory abilities.
These cells are enriched with Toll-like receptor 5 (TLR5), a well-known pattern recognition receptor in the immune system. TLR5 selectively recognizes bacterial flagellin, the principal protein component of bacterial flagella—a highly conserved structure across numerous bacterial taxa.
Intriguingly, the expression of TLR5 increases along the gut from the ileum to the distal colon, peaking where microbial density is highest, implying these cells play a crucial role in host-microbe interactions.
Experimental Findings: The Role of TLR5 in Appetite Regulation
To probe the functional role of TLR5 on neuropod cells, the team engineered mice with a conditional knockout of TLR5 specifically in these cells. Compared to normal controls, these mice consumed more food and gained significantly more weight; female mice also exhibited longer durations of feeding.
Crucially, neither metabolic parameters (such as glucose tolerance or fasting blood glucose) nor inflammation markers were altered, indicating that the observed changes were independent of systemic metabolic dysfunction or immune activation.
Further investigation revealed the mechanism at play: binding of bacterial flagellin to TLR5 on neuropod cells triggered intracellular calcium signaling, which in turn stimulated the release of the peptide YY (PYY). PYY is a potent enteroendocrine hormone known to suppress appetite by acting on receptors in the vagal ganglia — a neural junction in the gut-brain axis.
Consistent with these findings, mice allowed to feed ad libitum exhibited elevated levels of flagellin in feces compared with fasted mice. Moreover, direct administration of flagellin into the colon of healthy mice rapidly reduced food intake within 20 minutes. This effect was abolished in mice lacking TLR5, underscoring the receptor’s critical role.
Implications for Appetite Control and Beyond
This discovery reveals an elegant feedback loop whereby an increase in bacterial flagellin levels post-prandially alerts neuropod cells to release PYY, which then signals the brain via the gut-brain axis to curb feeding. It presents a novel “neurobiotic sense” that expands the repertoire of human sensory modalities to include real-time microbial pattern detection.
Understanding this gut sensory system has broad implications. It may help explain how dietary changes influence appetite and body weight through microbial shifts. Furthermore, it opens new avenues for therapeutic interventions targeting neuropod cells, TLR5 pathways, or PYY signaling for obesity and metabolic disorders.
Future Questions and Perspectives
This research also prompts intriguing questions: Could the brain manipulate this sensory feedback to selectively cultivate beneficial microbiota? Might this axis influence mood, cognition, or other gut-brain mediated behaviors?
Further studies are needed to explore whether similar mechanisms exist in humans and how environmental or genetic factors modulate this sensory system.
Expert Insights
Dr. Sarah Thompson, a gastroenterologist not involved in the study, comments, “This work beautifully highlights the complex crosstalk between our gut microbes and nervous system. It changes how we view appetite regulation—from a brain-centric to a more integrated brain-gut-microbiome perspective.”
Patient Scenario
Sarah, a 38-year-old woman struggling with weight management despite diet and exercise, might benefit from emerging knowledge about her gut’s neurobiotic sense. Understanding how microbial interactions modulate her hunger and satiety signals could guide future personalized interventions, possibly using probiotics or targeted therapies to optimize her gut-brain signaling and improve appetite control.
Conclusion
The identification of a “neurobiotic sense” in the gut marks a major advance in sensory science and metabolism research. It exemplifies the intimate dialogue between host and microbiota in regulating feeding behavior, with potential impacts for tackling obesity and metabolic diseases.
As research unfolds, integrating this sensory axis into clinical practice could revolutionize how we approach appetite disorders and harness the microbiome for health.
References
1. Liu WW, Reicher N, Alway E, et al. A gut sense for a microbial pattern regulates feeding. Nature. 2025. https://doi.org/10.1038/s41586-025-09301-7
2. Cani PD. Gut microbiota and obesity: lessons from the microbiome. Brief Funct Genomics. 2013;12(4):381-387. doi:10.1093/bfgp/elt016
3. Yadav H, Lee JH. Gut microbial metabolites as a key to regulating metabolic health. Trends Endocrinol Metab. 2019;30(3):196-205. doi:10.1016/j.tem.2018.12.006
4. Carbone F, La Rocca C, Matarese G. Immunomodulatory effects of leptin in the pathogenesis and progression of autoimmune diseases. J Immunol. 2015;194(10):4546-4553. doi:10.4049/jimmunol.1401444