Background
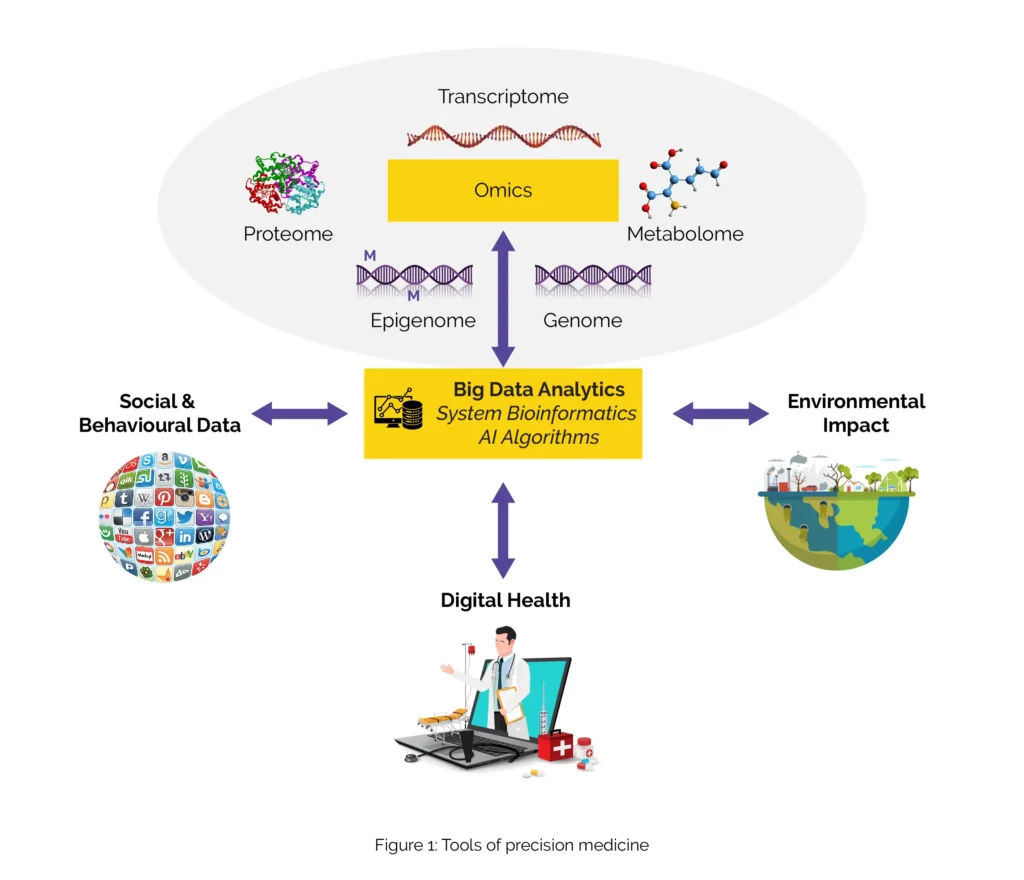
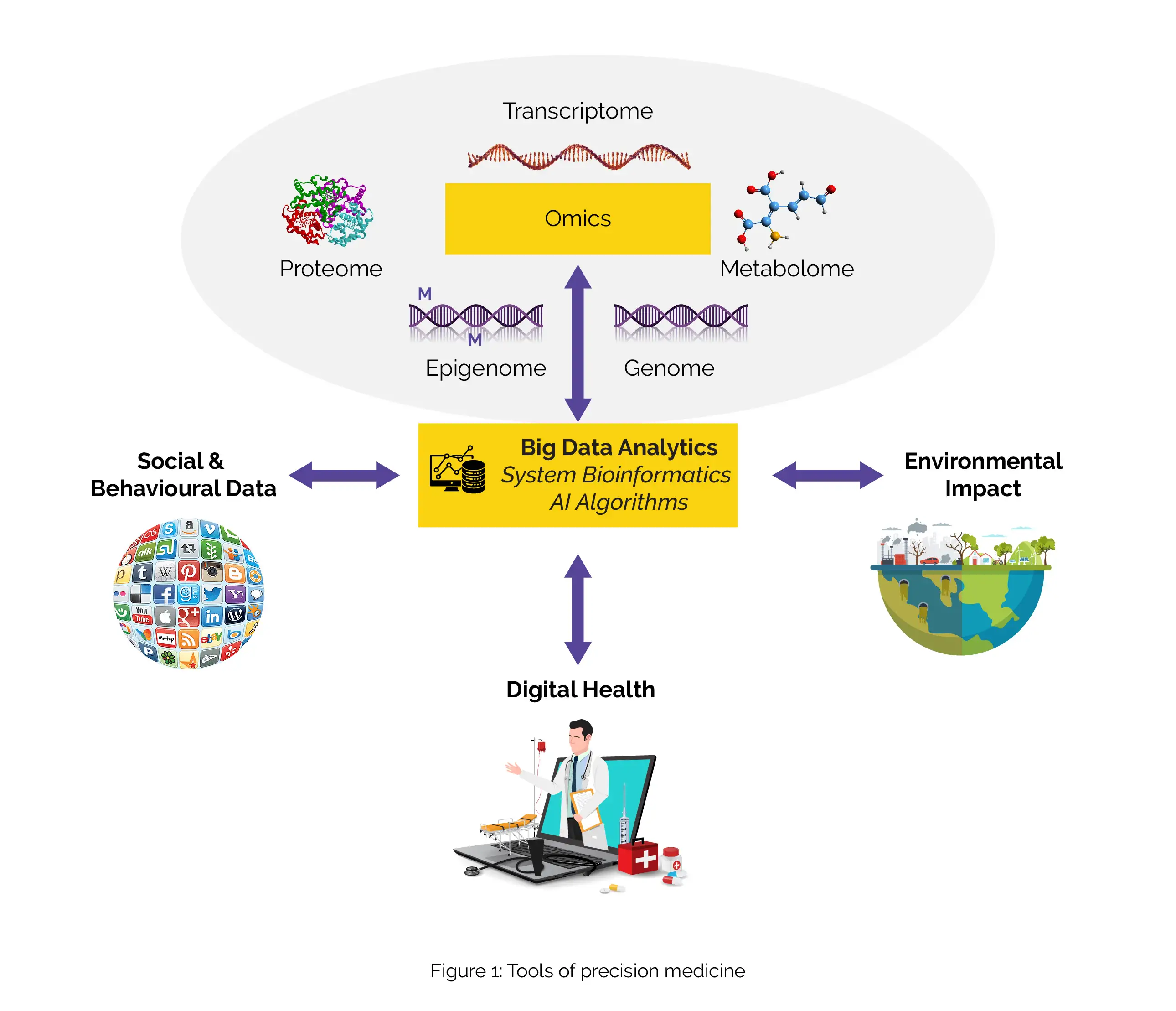
In recent years, the concept of personalized medicine has moved from the realm of science fiction into a rapidly growing reality. This approach to healthcare is fundamentally transforming how we treat and manage diseases by focusing on the unique genetic makeup of an individual. Personalized medicine leverages information about a person’s DNA to tailor medical treatments, making them more effective and reducing the risk of adverse effects.
Scientific and Clinical Evidence: What the Data Tell Us
The emergence of personalized medicine is backed by robust scientific evidence. Studies have shown that genetic variations can significantly impact how individuals respond to medications. For instance, some people may metabolize drugs faster, requiring higher doses for efficacy, while others may experience severe side effects from standard doses.
A landmark study published in the New England Journal of Medicine demonstrated how genetic testing could predict patient responses to warfarin, a commonly prescribed blood thinner. By analyzing specific genetic markers, researchers were able to tailor warfarin dosages to individual patients, improving safety and effectiveness.
Similarly, in oncology, genetic profiling is used to identify mutations in cancer cells, allowing clinicians to prescribe targeted therapies that attack cancer more precisely while sparing healthy cells. This approach not only enhances treatment efficacy but also minimizes toxic side effects.
Misconceptions and Harmful Behaviors
Despite its growing prominence, personalized medicine is often misunderstood. One common misconception is that it can provide a one-size-fits-all solution. In reality, while genetic testing offers valuable insights, it is only one piece of the puzzle. Environmental factors, lifestyle choices, and other medical conditions also play crucial roles in determining health outcomes.
There is also a risk of over-reliance on genetic information, leading to neglect of conventional medical practices that are equally important. Patients may misunderstand the capabilities of genetic tests, assuming they can predict all aspects of future health, which can lead to anxiety or inappropriate medical decisions.
Correct Health Practices and Practical Recommendations
For individuals considering personalized medicine, it is essential to consult healthcare professionals who are well-versed in genetics and personalized treatment plans. Genetic testing should be viewed as part of a comprehensive approach to health, complementing other diagnostic tools and lifestyle assessments.
Patients should engage in open discussions with their healthcare providers about the benefits and limitations of genetic testing. It is equally important to maintain a balanced lifestyle, including diet, exercise, and regular check-ups, which all contribute to overall health.
Expert Insights and Commentary
Dr. Emily Carter, a leading geneticist at the Institute of Personalized Medicine, emphasizes the revolutionary impact of personalized treatments. “We are witnessing a paradigm shift in healthcare,” she says. “By understanding the genetic blueprint of a patient, we can design treatments that are not only more effective but also safer, reducing trial-and-error approaches.”
Dr. Carter also notes the importance of educating both healthcare providers and patients about genetic literacy. “Understanding genetic risks and variations is crucial. It empowers patients and clinicians to make informed health decisions,” she adds.
Conclusion
Personalized medicine is undoubtedly a transformative force in modern healthcare. By harnessing the power of genetic information, it offers a promising pathway to more precise and effective treatment strategies. However, it is vital to approach this innovation with a balanced perspective, integrating genetic insights with traditional medical practices.
As the field continues to evolve, ongoing research and collaboration between geneticists, clinicians, and patients will be integral in realizing the full potential of personalized medicine, paving the way for a future where treatments are as unique as the individuals they serve.
References
1. Johnson, J. A., et al. (2017). Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for Pharmacogenomics-Guided Warfarin Dosing: 2017 Update. Clinical Pharmacology & Therapeutics.
2. Collins, F. S., & Varmus, H. (2015). A New Initiative on Precision Medicine. New England Journal of Medicine.
3. Veeck, J., & Esteller, M. (2010). Breast Cancer Epigenetics: From DNA Methylation to MicroRNAs. Journal of Mammary Gland Biology and Neoplasia.