Highlights
- West Nile virus (WNV) is the most prevalent mosquito-borne disease in the contiguous United States, causing over 1,200 neuroinvasive cases and 120 deaths annually.
- Transmission is primarily via Culex mosquitoes, but rare cases occur through blood transfusion, organ transplantation, and other routes.
- No effective antiviral therapy or human vaccine exists; prevention relies on personal protection and community mosquito control measures.
- Older adults and immunocompromised individuals, including those with hematologic malignancies and transplant recipients, are at highest risk for severe disease and long-term sequelae.
Clinical Background and Disease Burden
West Nile virus (WNV), a neurotropic flavivirus, was first detected in the Western Hemisphere in 1999 and has since become endemic in the United States. WNV is now the leading cause of mosquito-borne disease in the contiguous U.S., with an annual mean of 1,298 neuroinvasive disease cases and 129 deaths reported from 2014 to 2023. Neuroinvasive disease, including meningitis, encephalitis, and acute flaccid myelitis, is associated with significant morbidity and mortality. Notably, up to 80% of WNV infections are asymptomatic, while 20% cause West Nile fever (a mild, self-limited febrile illness), and less than 1% progress to neuroinvasive forms. Disproportionate burden falls on the elderly and immunocompromised, with mortality rates rising to 20% in those aged 70 or older and up to 40% in immunosuppressed populations.
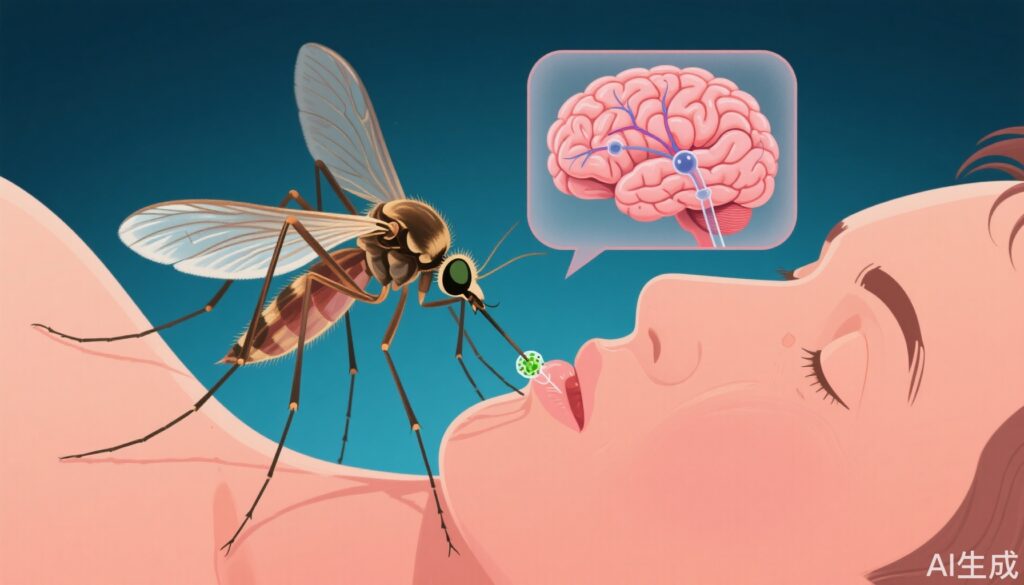
Transmission Dynamics and Epidemiology
The primary mode of WNV transmission is via the bite of infected Culex species mosquitoes. Rare non-vector transmission routes include blood transfusion, organ transplantation, transplacental, perinatal, breastmilk, and, less commonly, percutaneous or conjunctival exposure. Surveillance data reveal episodic outbreaks, with significant clusters reported in Europe, Tunisia, Israel, and the U.S. since 2018. In 2021, Maricopa County, Arizona, recorded the largest U.S. county-level outbreak with 1,487 cases and 101 deaths, underscoring the potential for localized epidemics.
Clinical Manifestations
WNV infection spectrum ranges from asymptomatic seroconversion to severe neurological disease. West Nile fever typically presents with abrupt onset of fever, headache, myalgia, and occasionally rash. Neuroinvasive disease manifests as meningitis, encephalitis, or acute flaccid myelitis, with symptoms such as altered mental status, focal neurologic deficits, and flaccid paralysis. Among those hospitalized for neuroinvasive disease, 30–40% require long-term care, and over 50% experience persistent sequelae, including fatigue, weakness, cognitive impairment, and depression.
Diagnostic Approach
Clinical suspicion for WNV should be heightened in patients presenting with fever or neurologic symptoms during the summer and fall months, particularly in endemic regions. Laboratory diagnosis is typically achieved through detection of WNV-specific IgM antibodies in serum or cerebrospinal fluid (CSF). Confirmatory neutralizing antibody tests are recommended in cases of potential cross-reactivity with other flaviviruses, atypical presentations, fatalities, or suspected non-mosquito transmission (such as organ transplantation). In severely immunocompromised patients, reverse transcription–polymerase chain reaction (RT-PCR) testing may offer higher sensitivity, given attenuated antibody responses.
Case Vignette
Mr. John Carter, a 72-year-old kidney transplant recipient from Arizona, presented in mid-August with fever, confusion, and limb weakness. CSF analysis revealed pleocytosis, and WNV IgM was positive. He required intensive care, and after prolonged hospitalization, was discharged to a rehabilitation facility with persistent motor deficits, illustrating the high risk and severe impact of WNV neuroinvasive disease in immunocompromised elderly patients.
Mechanistic Insights
WNV is neurotropic, capable of crossing the blood-brain barrier and infecting neurons, leading to inflammation and cell death within the central nervous system. Immunocompromised hosts are particularly susceptible due to impaired B-cell and T-cell responses. Recent studies highlight the particular vulnerability of patients on B-cell–depleting monoclonal antibodies and solid organ transplant recipients.
Prevention and Control Strategies
No antiviral therapies or vaccines are currently approved for human use. Preventive efforts focus on:
- Personal protective measures: consistent use of EPA-registered mosquito repellents, wearing long-sleeved clothing, and limiting outdoor activity during peak mosquito hours (dusk to dawn).
- Environmental management: elimination of standing water, larviciding, and adulticiding in communities.
- Blood and organ donor screening: all blood donations in the U.S. are screened for WNV since 2003, dramatically reducing transfusion-associated transmission.
- Public health surveillance: ongoing monitoring and rapid response to outbreaks.
Controversies and Limitations
A major challenge in WNV management is the absence of effective therapeutic agents or vaccines, despite decades of research. The unpredictable nature of outbreaks complicates targeted public health interventions. Diagnostic limitations in immunosuppressed patients can delay recognition and management. Long-term sequelae remain underappreciated, with few structured rehabilitation programs for survivors.
Conclusion
West Nile virus remains a significant public health concern in the U.S., with sustained annual morbidity and mortality. Older adults and immunocompromised individuals are at greatest risk for severe disease and long-term disability. With no effective therapy or vaccine available, clinicians and public health authorities must prioritize preventive strategies, early clinical recognition, and robust surveillance. Ongoing research into vaccines and novel therapeutics is urgently needed.
References
1. Gould CV, Staples JE, Guagliardo SAJ, Martin SW, Lyons S, Hills SL, Nett RJ, Petersen LR. West Nile Virus: A Review. JAMA. 2025 Jul 7. doi: 10.1001/jama.2025.8737 IF: 55.0 Q1 .2. Petersen LR, Brault AC, Nasci RS. West Nile virus: review of the literature. JAMA. 2013;310(3):308–315. doi:10.1001/jama.2013.8042 IF: 55.0 Q1 .3. Sejvar JJ. Clinical manifestations and outcomes of West Nile virus infection. Viruses. 2014;6(2):606–623. doi:10.3390/v6020606 IF: 3.5 Q2 .