Highlight
Volenrelaxin, despite its hypothesized benefits as a long-acting relaxin analog, demonstrated only dose-dependent improvement in left atrial (LA) reservoir strain at the lowest dose in patients with recently decompensated HFpEF. Paradoxically, treatment was associated with increased NT-proBNP levels, a marker of congestion, without beneficial effects on kidney function. Safety signals indicated a trend toward increased heart failure hospitalizations and more serious cardiovascular and renal adverse events, leading to early trial termination.
Study Background and Disease Burden
Heart failure with preserved ejection fraction (HFpEF) is a complex syndrome characterized by signs and symptoms of heart failure despite a normal or near-normal left ventricular ejection fraction. It constitutes about half of all heart failure cases and carries a substantial morbidity and high healthcare burden. Patients often exhibit circulatory congestion due to elevated filling pressures, which worsens symptoms and predisposes to frequent hospitalizations. Current therapies have limited efficacy in reducing congestion and improving outcomes in HFpEF.
Relaxin, a naturally occurring peptide hormone, has vasodilatory, antifibrotic, and diuretic properties, and has been proposed as a therapeutic agent to improve circulatory congestion and kidney function in heart failure. Volenrelaxin, a long-acting human relaxin formulation, offers the potential to sustain these benefits. Prior small-scale studies suggested possible hemodynamic improvements, making it a promising candidate for targeted HFpEF therapy.
Study Design
This international, multicenter, double-blinded, phase 2 randomized controlled trial enrolled 332 patients with New York Heart Association (NYHA) class II-IV HFpEF who had recent heart failure decompensation. Participants were randomized to receive subcutaneous weekly injections of volenrelaxin at 25 mg, 50 mg, 100 mg, or placebo.
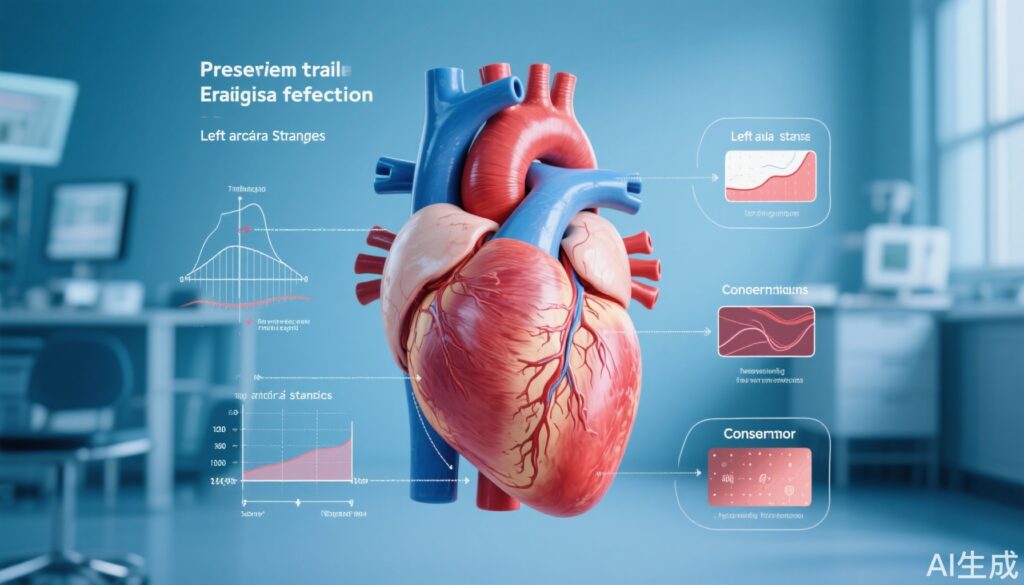
The primary endpoint was the change in left atrial (LA) reservoir strain—a sensitive echocardiographic marker of LA compliance and function—at 26 weeks. Key secondary endpoints included changes in biomarkers of congestion (N-terminal pro-B-type natriuretic peptide, NT-proBNP), kidney function assessed by estimated glomerular filtration rate (eGFR), and safety/tolerability.
The trial was terminated early by the sponsor due to emerging evidence of worsening congestion among treated patients.
Key Findings
At 26 weeks, administration of the lowest dose volenrelaxin (25 mg) was associated with a statistically significant improvement in LA reservoir strain compared to placebo (+3.9%, 95% CI: 1.1 to 6.6, P = 0.006). However, this effect was not observed at the 50 mg (+1.3%, 95% CI: -1.3 to 3.9, P = 0.332) or 100 mg (+0.9%, 95% CI: -1.8 to 3.6, P = 0.521) doses, indicating a lack of dose-response relationship.
Contrary to expectations, volenrelaxin treatment across all doses led to a 24.5% increase in NT-proBNP levels (95% CI: 2.0% to 51.8%) at 26 weeks relative to placebo. NT-proBNP elevation is a biomarker indicative of increased cardiac wall stress and congestion, suggesting a paradoxical worsening of volume status despite modest improvement in LA function at low dose.
No significant effect on kidney function was detected, with eGFR changes being non-significant (+2.2 ml/min/1.73 m², 95% CI: -1.8 to 6.3).
Safety analyses revealed a trend toward increased risk of heart failure hospitalization in the volenrelaxin group compared to placebo (hazard ratio 2.64, 95% CI: 0.93 to 7.56, P = 0.070). Additionally, there was a near-significant increase in cardiovascular and renal serious adverse events (odds ratio 2.52, 95% CI: 0.95 to 6.68, P = 0.056).
The study cohort had a mean age of 74 years, nearly equal gender distribution (49% women), mean body mass index of 30.6 kg/m², and 31.9% were NYHA class III-IV, reflecting a representative population with advanced HFpEF.
Expert Commentary
This trial provides important insights and a cautionary message regarding the therapeutic use of long-acting relaxin analogs in HFpEF. While the improvement in LA reservoir strain at the lowest dose indicates some beneficial impact on atrial compliance, the lack of dose-dependence and concurrent NT-proBNP elevation point to complex, possibly opposing physiological effects of volenrelaxin.
The increased congestion and suggestion of worse clinical outcomes raise concerns about the mechanisms by which volenrelaxin interacts with cardiac and renal physiology in this vulnerable population. Potential off-target effects, altered vascular permeability, or maladaptive neurohormonal activation might underlie these findings.
Limitations include early trial termination limiting longer-term data, the relatively small sample size for safety endpoint conclusions, and the absence of detailed mechanistic assessments to clarify the inconsistency between LA function and congestion markers. Future studies should explore these pathways and carefully evaluate dosing and patient subgroups.
Conclusion
In summary, volenrelaxin—a promising candidate based on its biological rationale—did not confer overall clinical benefit in HFpEF patients, with signals for harm including worsening congestion and increased adverse events. Despite some improvement in left atrial strain at the lowest dose, this therapy should not be pursued further without a deeper understanding of its complex effects on heart failure pathophysiology.
These findings underscore the challenges of drug development in HFpEF and the need for cautious evaluation of novel agents affecting the delicate balance of cardiac, vascular, and renal function in this heterogeneous syndrome.
References
Borlaug BA, Testani JM, Petrie MC, Wang Z, Cunningham J, Adams KF Jr, Amir O, Bělohlávek J, Bocchi E, Freitas A Jr, Hominal M, Kadokami T, Merkely B, Miller CA, Nuñez J, Verma S, Yilmaz MB, Oru E, Sam F. Effects of volenrelaxin in worsening heart failure with preserved ejection fraction: a phase 2 randomized trial. Nat Med. 2025 Aug 31. doi: 10.1038/s41591-025-03939-6. Epub ahead of print. PMID: 40887551.