Introduction and Clinical Context
Pediatric asthma remains a significant public health challenge worldwide, especially in urban, low-income populations. Despite advances in biologic therapies targeting type 2 (T2) inflammation, such as mepolizumab, a subset of children continue to experience residual exacerbations. Mepolizumab, an anti-interleukin-5 monoclonal antibody, effectively reduces eosinophilic inflammation and associated exacerbation risk; however, it does not eliminate all exacerbations, indicating underlying heterogeneity in inflammatory mechanisms. Understanding these residual inflammatory pathways is crucial for developing comprehensive management strategies and personalized therapies, particularly in vulnerable urban pediatric populations where exacerbations contribute to morbidity and healthcare burden.
Study Design and Methodology
The analysis was conducted as a secondary study embedded within the MUPPITS-2 trial—a randomized, double-blind, placebo-controlled, parallel-group clinical trial involving 290 children aged 6-17 years with exacerbation-prone asthma residing in urban low-income settings across nine U.S. cities. Participants received subcutaneous mepolizumab (40 mg for children 6-11 years, 100 mg for those 12-17 years) or placebo every four weeks over 52 weeks. During acute respiratory illnesses recorded in the trial, nasal samples were collected for transcriptomic analysis via RNA sequencing. The primary endpoint involved identifying transcriptional signatures associated with exacerbations, compared between treatment groups and illness types, and correlated with pulmonary function data.
Major Findings and Results
The study analyzed 176 acute respiratory illness events in 108 children, with 63 episodes resulting in exacerbations. Key findings include:
- Children receiving mepolizumab showed significant downregulation of an eosinophil-associated T2 inflammation module during exacerbations (log2 fold change of -0.60; false discovery rate [FDR] < 0.05). This aligns with expected effects of eosinophil depletion but indicates residual inflammatory activity persists.
- Contrarily, increased expression was observed in gene modules linked to epithelial and macrophage inflammatory pathways (log2 FC estimates ranged from 0.22 to 0.85; FDR < 0.05), suggesting alternative inflammatory axes independent of eosinophils.
- Both groups exhibited upregulated mucus secretion and cellular stress response pathways during exacerbations compared to nonexacerbation illnesses, highlighting common pathways involved in respiratory distress.
- Notably, epithelial inflammatory pathway activation persisted in the mepolizumab group irrespective of viral presence, whereas macrophage pathway activation was significantly associated with viral-induced exacerbations.
- Three semiorthogonal inflammatory axes—eosinophil/T2 inflammation, epithelial stress, and macrophage activation—were identified as independently contributing to heterogeneity among exacerbations.
These findings underscore the complexity of residual airway inflammation, involving multiple, overlapping biological pathways beyond traditional eosinophilic mechanisms. The data imply that targeting eosinophils alone is insufficient to prevent all exacerbations and that distinct inflammatory axes can operate independently or synergistically, influenced by viral infections and epithelial responses.
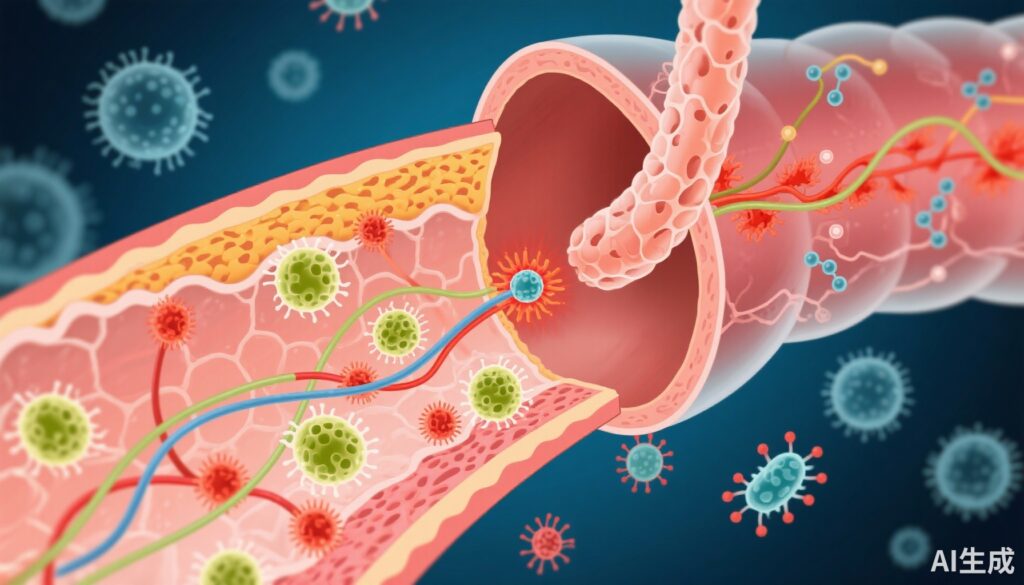
Mechanistic Insights and Biological Relevance
The persistence of epithelial and macrophage-driven inflammation in children on mepolizumab suggests alternative pathways may sustain or trigger exacerbations. Epithelial cells, fundamental to airway barrier integrity, can release cytokines and chemokines that recruit and activate immune cells, propagating inflammation even in eosinophil-depleted environments. Likewise, macrophages, as key innate immune regulators, can respond robustly to viral infections, fostering inflammatory cascades independent of eosinophil activity.
These pathways may involve cytokines such as IL-8, GM-CSF, and others, promoting mucus hypersecretion and cellular stress responses observed during exacerbations. The independence of these axes from viral infections in epithelial inflammation indicates potential intrinsic activation rather than solely infection-driven processes, emphasizing their biological plausibility and relevance in residual asthma exacerbations.
Implications for Clinical Practice and Future Research
The findings highlight the necessity for multi-targeted approaches in asthma management, especially for patients on eosinophil-directed biologics. Therapeutic strategies that concurrently modulate epithelial dysfunction, macrophage activity, and mucus secretion may reduce residual exacerbations more effectively. Development of biomarkers capable of identifying dominant inflammatory axes could facilitate personalized treatment, optimizing outcomes.
Further research is needed to elucidate molecular drivers of these pathways and assess novel therapeutics targeting epithelial integrity and macrophage responses. The potential for combinatorial biologic therapies or small molecules to address heterogeneity in inflammatory mechanisms offers promising avenues for advancing pediatric asthma care.
Study Limitations and Generalizability
While providing valuable insights, the study’s limitations include reliance on nasal transcriptomics as a surrogate for lower airway inflammation, which may not perfectly reflect bronchial processes. Additionally, the urban, low-income cohort may limit generalizability to other populations. Larger, diverse cohorts with invasive airway sampling could strengthen the understanding of these mechanisms.
Conclusion
Residual asthma exacerbations in children treated with mepolizumab involve multiple distinct inflammatory pathways beyond eosinophils, notably epithelial and macrophage-driven mechanisms. Recognizing this heterogeneity is essential for developing comprehensive and personalized therapeutic strategies aimed at reducing exacerbation burden and improving long-term disease control in pediatric asthma.