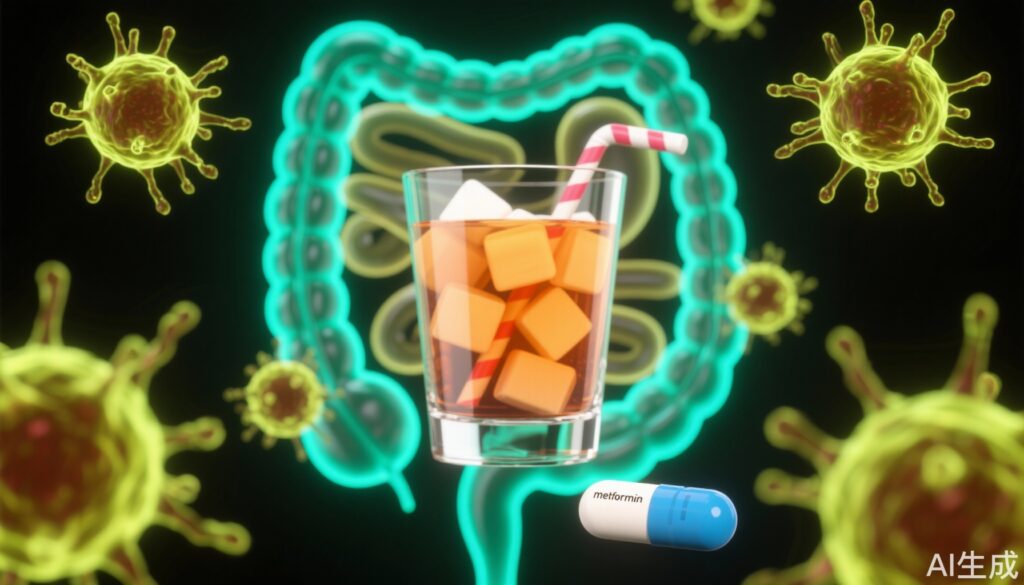
Introduction: The Hidden Consequences of Excess Fructose in Our Diets
Sugary drinks such as bubble tea, soda, fruit juice, and processed foods ubiquitously contain fructose—a sweetener prized for its high sweetness and low cost. Once thought to be just an innocent source of extra calories, fructose has increasingly been implicated as a major contributor to obesity, fatty liver disease, and type 2 diabetes. More alarmingly, recent research indicates that fructose might also quietly “ignite” the immune system, exacerbating chronic inflammation, especially in inflammatory bowel diseases (IBD) like Crohn’s disease and ulcerative colitis.
Researchers from Sichuan University’s West China School of Medicine have just uncovered a surprising and concerning mechanism through which high fructose intake directly affects the immune system. Their findings reveal that fructose stimulates key immune players—pro-inflammatory T helper cell subtypes Th1 and Th17—in ways that worsen intestinal inflammation. Notably, this process occurs independently of gut microbiota changes or metabolic syndrome, instead depending on intracellular signaling pathways within immune cells themselves.
What the Data Tell Us: Fructose’s Direct Impact on T Cells and Gut Inflammation
For years, scientists have known that fructose could indirectly influence health by altering the gut microbiome or disrupting liver metabolism. However, whether fructose could directly regulate the adaptive immune system, especially T cells, was unclear. Most literature suggested that T cells lacked the fructose transporter protein GLUT5 and thus couldn’t effectively take up fructose.
This new study challenges this notion. Experimental data show that although T cells do not directly “consume” fructose, fructose enhances glutamine metabolism within T cells—a key pathway feeding into immune cell activation. This metabolic reprogramming activates mTORC1, a critical cellular “growth switch.” Once activated, mTORC1 drives CD4+ T cells to differentiate into Th1 and Th17 cells, the very cells responsible for perpetuating chronic inflammation and autoimmune disease.
Th1 cells produce interferon-gamma (IFN-γ), triggering a potent cell-mediated immune response, while Th17 cells secrete interleukin-17A (IL-17A), which, although protective against infection, can cause severe tissue damage and ongoing inflammation. In mouse models consuming 20% fructose water for two months, researchers observed a significant increase in Th1 and Th17 cells in intestinal tissue, spleen, and mesenteric lymph nodes, without a compensatory rise in regulatory T cells (Tregs) that usually help maintain immune balance. This imbalance shifts the immune system into an overactive, damaging state.
Mechanistic Insights: The Double Whammy of ROS and TGF-β Activation
Further investigations revealed fructose elevates reactive oxygen species (ROS) inside T cells. Increased ROS activates latent transforming growth factor-beta (TGF-β), a cytokine instrumental in promoting Th17 cell generation. Through this dual mechanism—metabolic reprogramming and oxidative stress—fructose acts as an “invisible accelerator” of intestinal inflammation.
Metformin: A Surprise Ally in Combating Fructose-Induced Inflammation
Perhaps the most hopeful finding is that metformin, a drug widely used for type 2 diabetes, effectively counters fructose-induced immune dysfunction. Metformin inhibits mTORC1 activation, thus blocking fructose-triggered Th1 and Th17 differentiation. Simultaneously, it lowers ROS levels and curbs the abnormal activation of TGF-β, thereby reducing inflammatory T cell expansion.
In mouse models of colitis fed high fructose, administering metformin significantly alleviated key disease features—weight loss was slowed, colon shortening reduced, and tissue inflammation markedly decreased. These results suggest metformin not only controls blood sugar but also possesses potent immunomodulatory properties beneficial for treating or preventing inflammation-driven diseases linked to high fructose intake.
Clinical and Public Health Implications
This groundbreaking research shifts the paradigm on fructose from being merely a high-calorie dietary component to a direct modulator of immune cell fate and function. It raises serious questions about the health consequences of widespread fructose consumption in modern diets.
People who regularly consume sugary beverages and processed foods, especially those at risk for inflammatory bowel diseases, may be unwittingly fueling latent immune imbalances. Current clinical guidance around sugar often emphasizes metabolic risks like obesity and diabetes, but this work highlights an equally important inflammatory dimension.
Practical Recommendations and Expert Insights
Experts recommend limiting consumption of high-fructose foods and beverages to reduce the risk of triggering immune-mediated inflammation. Given the results regarding metformin, there is growing interest in exploring its off-label application for patients prone to fructose-related inflammation, although human clinical trials are necessary to confirm safety and efficacy in this context.
Dr. Lisa Thompson, a gastroenterologist specializing in IBD, comments, “This study emphasizes the immune implications of diet beyond metabolism. It opens new avenues for integrative treatment strategies combining dietary modification and targeted pharmacology.”
Case Scenario: Sarah’s Journey with Inflammatory Bowel Disease and Diet
Sarah, a 28-year-old teacher, was diagnosed with ulcerative colitis. She frequently consumed sodas and fruit-flavored drinks high in fructose. Her condition worsened despite standard therapies. After dietary counseling to reduce high-fructose intake and initiating metformin, Sarah reported fewer flare-ups and improved quality of life. Although anecdotal, her case illustrates potential real-world benefits from the mechanisms uncovered by recent research.
Conclusion: Sweet Danger and a Path to Therapeutic Innovation
High fructose intake directly activates pro-inflammatory immune pathways by metabolic reprogramming of T cells, particularly boosting harmful Th1 and Th17 cells, which intensify intestinal inflammation linked to IBD. Metformin offers a promising method to reverse these effects by targeting mTORC1 signaling and oxidative stress.
While still based on animal studies, this research provides clear mechanistic insight and a compelling rationale for limiting fructose consumption as part of preventing or managing chronic inflammatory diseases.
As modern diets continue to flood the body with fructose, it’s crucial to recognize that this sweet ingredient may awaken an “immune storm” inside us. Future strategies involving diet modulation and metabolic drugs like metformin hold promise for personalized health management against inflammatory conditions.
References
Ma, X., Chen, J., Wang, F. et al. High fructose consumption aggravates inflammation by promoting effector T cell generation via inducing metabolic reprogramming. Signal Transduction and Targeted Therapy 10, 271 (2025). https://doi.org/10.1038/s41392-025-02359-9