Highlights
- The two-step clinical care pathway (FIB-4 followed by VCTE) effectively stratifies metabolic dysfunction-associated steatotic liver disease (MASLD) patients by risk of liver-related events.
- Over 80% of patients can be safely classified as low-risk using this efficient, noninvasive strategy, reserving additional testing for a minority.
- This approach maintains high prognostic accuracy (time-dependent AUC 0.840) and supports rational allocation of healthcare resources.
- Alternative second-step tools (Agile, FAST scores) did not significantly improve predictive performance over VCTE-based liver stiffness measurement.
Clinical Background and Disease Burden
Metabolic dysfunction-associated steatotic liver disease (MASLD, formerly known as NAFLD) has emerged as the leading cause of cirrhosis and hepatocellular carcinoma globally, now affecting more than 30% of the general population. Given the vast number of individuals with MASLD, but the reality that only a small proportion will progress to severe complications such as liver failure or cancer, accurate and cost-effective risk stratification is a major unmet need, especially as most MASLD patients are managed in primary care settings rather than hepatology specialty clinics.
In 2021, the American Gastroenterological Association (AGA) endorsed a two-step risk stratification pathway: initial screening with the Fibrosis-4 Index (FIB-4), followed by liver stiffness measurement (LSM) via vibration-controlled transient elastography (VCTE) for patients with intermediate FIB-4 values. However, the real-world prognostic validity and clinical efficiency of this approach required rigorous multinational evaluation.
Research Methodology
This prospective cohort study, published by Yip et al. in the Journal of Hepatology, enrolled 12,950 adult MASLD patients from 16 centers across the United States, Europe, and Asia between February 2004 and January 2023. Fourteen centers contributed prospective data. Inclusion criteria required histologic or imaging confirmation of hepatic steatosis, available FIB-4 and VCTE results, and exclusion of other chronic liver diseases (e.g., viral hepatitis, HIV) or prior advanced liver events.
At each clinical encounter, patient histories, body mass index (BMI), blood tests (liver biochemistry, renal function, hematology, glucose, lipids), and liver stiffness (via FibroScan, Echosens) were collected. FIB-4, Agile, and FAST scores were calculated using established equations.
The primary endpoint was a composite of liver-related events: hepatocellular carcinoma, decompensated liver failure (ascites, variceal bleeding, hepatic encephalopathy, hepatorenal syndrome), liver transplantation, and liver-related death. Secondary endpoints included hepatocellular carcinoma and decompensation analyzed separately.
Risk stratification followed the AGA pathway: all patients underwent FIB-4 testing; those with FIB-4 between 1.3 (or 2.0 if age >65) and 2.67 received VCTE. Liver stiffness thresholds of 8 and 12 kPa further delineated risk. The study also explored alternative two-step algorithms using different cutoffs or substituting Agile and FAST scores for VCTE.
Key Findings
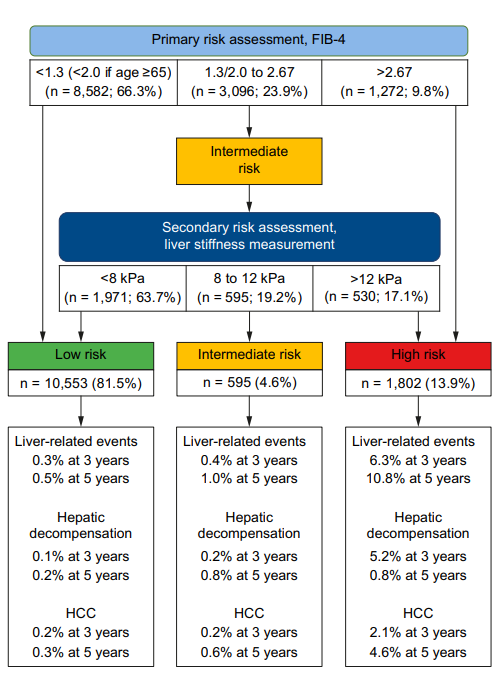
Of the 12,950 MASLD patients, initial FIB-4 stratification yielded 66.3% low-risk, 23.9% intermediate-risk, and 9.8% high-risk groups. After VCTE for intermediate-risk patients, 81.5% were classified as low-risk, 4.6% as intermediate, and 13.9% as high-risk.
Over a median follow-up of 47 months, 248 patients (1.9%) experienced liver-related events. Five-year cumulative incidence rates for liver-related events were:
- Low-risk: 0.5%
- Intermediate-risk: 1.0%
- High-risk: 10.8%
The two-step pathway demonstrated robust prognostic performance with a time-dependent AUC of 0.840 (95% CI 0.798–0.879). This approach significantly improved identification of high-risk patients compared to FIB-4 alone, guiding more targeted clinical interventions. Substituting Agile or FAST scores for VCTE in the second step did not further enhance prognostic accuracy. Adjusting VCTE thresholds (e.g., 10/15 kPa) modestly reduced the size of the intermediate-risk group but did not improve overall predictive performance.
Importantly, low-risk patients (over 80% of the cohort) had extremely low 5-year rates of severe hepatic outcomes, supporting a conservative management approach in primary care. High-risk patients had a more than 20-fold greater risk of events, justifying referral for specialist evaluation and intensified surveillance/intervention.
Case Vignette: Clinical Relevance
Consider Mr. John Miller, a 59-year-old man with obesity and type 2 diabetes, incidentally found to have hepatic steatosis. His FIB-4 score is 1.9 (intermediate risk). VCTE reveals liver stiffness of 14 kPa, classifying him as high-risk; this prompts referral to hepatology, advanced fibrosis assessment, and tailored surveillance for complications. Without the two-step pathway, he might have remained under-monitored in primary care, missing an opportunity for early intervention.
Expert Commentary
Current international guidelines (AGA, EASL) increasingly favor integrated, noninvasive risk stratification for MASLD. This study provides robust, multinational evidence validating the two-step FIB-4/VCTE pathway, streamlining care and reducing unnecessary referrals. As summarized by Yip et al., “Our findings support the two-step algorithm as an effective means to optimize MASLD management on both population and individual levels.”
Controversies and Limitations
Limitations include the observational design, potential selection bias (patients undergoing VCTE may differ from the broader MASLD population), and regional practice variations. The majority of patients were managed at tertiary centers, potentially limiting generalizability to purely primary care settings. Furthermore, the study excluded those with prior decompensation or cancer, so results may not extrapolate to all MASLD patients. The sensitivity of VCTE can be reduced in patients with obesity or technical limitations.
Conclusion
This large, rigorous, multinational study demonstrates that the two-step FIB-4 followed by VCTE algorithm is a highly effective, evidence-based method for risk stratifying MASLD patients in routine clinical practice. By safely identifying low-risk individuals and prioritizing resources for those at highest risk, this approach supports precision medicine, more efficient healthcare delivery, and improved patient outcomes. Future research may focus on refining risk thresholds for diverse populations and integrating novel noninvasive biomarkers or imaging modalities.
References
- Yip, Terry Cheuk-Fung, et al. “Prognostic performance of the two-step clinical care pathway in metabolic dysfunction-associated steatotic liver disease.” Journal of Hepatology, Volume 83, Issue 2, 304–314.
- American Gastroenterological Association. “AGA clinical practice update on diagnosis and management of nonalcoholic fatty liver disease.” Gastroenterology. 2021;160(6):2091-2099.
- European Association for the Study of the Liver (EASL). “EASL Clinical Practice Guidelines on non-invasive tests for evaluation of liver disease severity and prognosis.” J Hepatol. 2021;75(3):659-689.