Introduction
Intensive care units (ICUs) provide acute, specialized care for patients with life-threatening illnesses through technically complex interventions. Approximately 20% of patients admitted to the ICU are near the end of life, underscoring the vital role of palliative care to address symptom burden, support complex decision making, and provide holistic family care.1–3 The ICU environment varies by subspecialty (e.g., cardiac, neuro, surgical) and institutional culture, necessitating adaptable palliative care approaches. Specialty palliative care involvement has been linked to improved outcomes including decreased ICU length of stay.4–11
This article outlines ten practical tips to guide palliative care clinicians working with ICU teams to optimize care delivery, foster collaboration, respect diverse patient experiences, and navigate challenges unique to critical care settings.
1. Build and Maintain Strong Relationships with ICU Clinicians and Interdisciplinary Teams
Successful palliative care consultation depends on trust and mutual respect with ICU clinicians and associated teams. ICU clinicians face high burnout rates and ethical stresses related to complex decision making.12–16 Palliative care consultants must understand the culture and phase of palliative care integration in the ICU to tailor their approach—from education and referral encouragement in early stages to collaborative comanagement and resource optimization as programs mature.17
2. Collaboratively Identify the Most Suitable Model of Palliative Care Delivery
Effective specialty palliative care delivery in the ICU ranges from referral-based consultations to embedded or full takeover models.18–21 Selection should be a shared decision between ICU and palliative care teams, considering individual patient and family needs, medication management, team communication systems, follow-up requirements, and responsible providers for different care components. Models should remain flexible to evolving clinical situations.
3. Enhance Primary Palliative Care Skills Among ICU Team Members
Given limited specialty workforce capacity,22 primary ICU clinicians need competency in symptom control, communication, surrogate decision support, and transitions of care.23,24 Palliative care consultants can support this by: disseminating educational resources (e.g., VitalTalk, CAPC modules), advocating integration of palliative care into curricula, providing patient and family educational tools, and fostering interdisciplinary champions for ongoing skill development.
4. Support Surrogate Decision Makers and Care Partners Experiencing Distress
Surrogates commonly face urgent and complex decisions about unfamiliar ICU therapies, which can provoke psychological distress and post-intensive care syndrome-family (PICS-family).25–29 Recent family-centered care guidelines recommend strategies such as ICU orientation programs, ICU diaries, emotional support using open-ended questions, involving families in bedside care, and referrals to allied professionals including social work, chaplaincy, art and music therapists, and child life specialists.30–41
5. Utilize Prior Advance Care Planning and Goals Discussions to Elicit Patient Values
Clarifying goals of care is a frequent consultative reason. Capturing prior documented advance care planning and goals conversations is essential to avoid family distress related to perceived poor communication.42,43 Consulting bedside nurses who have close family contact can provide additional insights.44 Structured family meetings using an ask-tell-ask format and shared decision-making frameworks help align treatment options with patient values and facilitate consensus.45–47
6. Respect Diverse Lived Experiences, Beliefs, and Preferences Especially Regarding End-of-Life Care
Serious illness outcomes and care preferences differ beyond racial/ethnic lines and are shaped by socioeconomic status, healthcare access, and culturally bound values.48–52 Eliciting culturally important factors—fears, financial concerns, mistrust, spiritual beliefs—through sensitive engagement enables truly patient-centered care respectful of individual needs, particularly around end-of-life rituals and treatment decisions.
7. Employ the Time-Limited Trial Framework to Manage Prognostic Uncertainty
Time-limited trials (TLTs) allow critical care teams and surrogates to jointly evaluate benefit versus burden of life-sustaining therapies over a defined period.53–56 The American Thoracic Society framework emphasizes phases of consideration, planning, support, and reassessment with broad team communication. Use of TLTs enhances prognostic alignment, relationship-building, and shared decision-making in ICU settings.
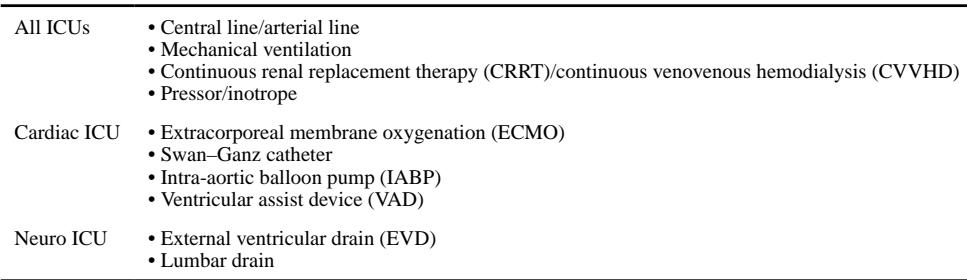
8. Ensure Optimal Symptom Management Prior to Withdrawal of Life-Sustaining Treatments
Symptom control is critical in withdrawal of support, requiring multidisciplinary collaboration to tailor plans based on patient physiology and dependency on modalities such as ECMO or ventilatory support.57,58 Stepwise withdrawal with careful opioid use for dyspnea and pain, appropriate anxiolytics, and testing of medication delivery routes ensures comfort throughout the process.
9. Use a Multimodal Approach to Resolve Intractable Conflicts Over Potentially Nonbeneficial Treatments
Disagreements between surrogates and clinicians about treatment appropriateness may lead to moral distress and excessive healthcare costs.59–64 A structured conflict resolution includes expert consultation, notifying surrogates about processes, obtaining second opinions, committee review, and providing opportunities for transfer or appeal where appropriate. Timely emotional support and transparent communication are crucial,
10. Develop a Proactive Follow-up Plan Post-ICU to Address Ongoing Palliative Needs
Transitions from ICU to wards or other settings are vulnerable periods often accompanied by uncertainty and stress.65,66 Many ICU survivors develop persistent critical illness or post-intensive care syndrome with ongoing physical and psychological symptoms, as do their caregivers.67,68 Palliative care teams should facilitate continuity by screening for high-risk patients, ensuring specialty consultation, and establishing workflows for inpatient and outpatient follow-up.
Conclusion
Delivering high-quality palliative care in the ICU requires deliberate, multifaceted strategies tailored to the unique patient, family, and ICU contexts. Building strong interdisciplinary relationships, choosing appropriate care delivery models, supporting surrogate decision makers, respecting diverse values, managing symptoms carefully, and navigating conflicts constructively all promote goal-concordant care. Structured communication tools like time-limited trials and coordinated transition planning further enhance patient and family outcomes in these highly complex settings.
References
Mehta A, Bullock K, Gustin JL, Hadler RA, Nelson JE, Rosa WE, Seaman JB, Varner-Perez SE, White DB. Top Ten Tips Palliative Care Clinicians Should Know About Intensive Care Unit Consultation. J Palliat Med. 2025 Aug 8:10.1177/10966218251366072. doi: 10.1177/10966218251366072. Epub ahead of print. PMID: 40780837; PMCID: PMC12395537.