Highlights
- Tongxinluo (TXL), a traditional Chinese medicine (TCM) compound, improves clinical outcomes in acute myocardial infarction (AMI), acute coronary syndrome (ACS), and ischemic stroke through multi-target mechanisms including anti-inflammatory, endothelial protective, and antiplatelet effects.
- Large randomized controlled trials (RCTs), such as the CTS-AMI trial, demonstrate that adjunctive TXL reduces 30-day and 1-year major adverse cardiac and cerebrovascular events (MACCEs) in ST-segment elevation myocardial infarction (STEMI) patients.
- Mechanistic studies elucidate TXL’s role in preserving endothelial barrier integrity via PPAR-α and angiopoietin-like 4 pathways, modulating platelet reactivity, and enhancing mesenchymal stem cell therapy efficacy through exosomal miRNA transfer.
- Clinical benefits are consistent across genetic subgroups such as CYP2C19 loss-of-function allele carriers, but gaps remain in robust evidence for long-term safety, effects in diverse populations, and specific mechanisms in different cardiovascular disease subtypes.
Background
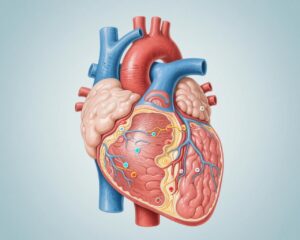
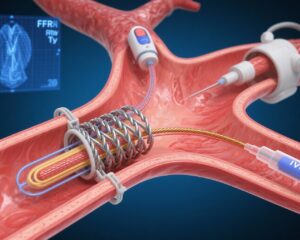
Cardiovascular diseases, including myocardial infarction, acute coronary syndrome, and ischemic stroke, remain leading causes of morbidity and mortality worldwide. Despite advances in revascularization techniques such as percutaneous coronary intervention (PCI), ischemia/reperfusion injury, no-reflow phenomena, and adverse remodeling limit optimal patient outcomes. Tongxinluo (TXL), a patented Chinese herbal compound, has been traditionally used for cardiovascular protection and microvascular repair. Recent decades have witnessed emerging preclinical and clinical data supporting its use as an adjunctive therapy, yet comprehensive synthesis of its mechanisms, clinical efficacy, and differential benefits across patient populations is lacking.
Key Content
Chronological Development of Evidence
The earliest mechanistic studies (circa 2005-2010) identified TXL’s endothelial protective effects in animal models of myocardial ischemia/reperfusion injury (MIRI), demonstrating attenuation of no-reflow by preserving endothelial integrity and regulating nitric oxide synthase activity (PMID: 19719943, 16313114). Concurrent clinical trials (ENLEAT trial, 2010) showed TXL reduced myocardial infarct size and no-reflow incidence post-emergency PCI in STEMI patients (PMID: 21034597). Subsequent clinical and mechanistic studies expanded understanding of TXL’s anti-inflammatory and antioxidant properties in endothelial cells and improvements in coronary microcirculation (PMID: 18625049, 27830021).
From 2011 to 2018, randomized studies in ACS and PCI populations illustrated TXL’s effects in reducing platelet activation markers (CD62P, CD63), improving endothelial function, and lowering inflammatory biomarkers such as high-sensitivity C-reactive protein (hsCRP) (PMID: 21608219, 29483383). Notably, a multicenter RCT reported enhanced platelet inhibition by TXL in ACS patients with high platelet reactivity (HPR), especially those carrying one CYP2C19 loss-of-function allele (PMID: 29483383).
The landmark CTS-AMI trial (2019-2021) was a large, multicenter, randomized, double-blind, placebo-controlled study enrolling nearly 3800 STEMI patients. TXL administered adjunctively with guideline-directed therapy significantly lowered 30-day MACCEs (RR 0.64, 95% CI 0.47–0.88) and cardiac death rates, with sustained benefit at one year (PMID: 37874574). Additionally, a large stroke RCT (2024) demonstrated improved 90-day functional outcomes with TXL in acute ischemic stroke patients (PMID: 39325453).
Mechanistic Insights and Translational Advances
TXL’s multifaceted protective effects include inhibition of inflammatory cytokine secretion from cardiac microvascular endothelial cells (PMID: 27830021), attenuation of ischemia/reperfusion injury via PPAR-α activation and induction of angiopoietin-like 4 to restore endothelial barrier integrity (PMID: 29912977), and antiplatelet activity reducing high platelet reactivity (PMID: 29483383).
Advanced cellular studies revealed TXL preconditioning enhances therapeutic efficacy of mesenchymal stem cells in myocardial repair, mediated by exosomal transfer of miR-146a-5p targeting IRAK1/NF-κB pathways, reducing apoptosis and inflammation post-AMI (PMID: 35799283, 35130979).
Network pharmacology and meta-analytical data identified 101 bioactive compounds in TXL acting on 149 targets, intersecting pathways like receptor ligand activity, AGE-RAGE signaling, and cellular senescence, which may underlie its effect in preventing coronary restenosis (PMID: 36743461).
Clinical Efficacy Across Disease Subtypes and Patient Populations
RCTs and meta-analyses support TXL’s role as an adjunct in STEMI, ACS, and ischemic stroke, improving symptom relief, cardiac function, and reducing recurrent ischemic events. Notably, TXL benefits extend to patients with genetically defined clopidogrel resistance (CYP2C19 LOF alleles), offering enhanced platelet inhibition (PMID: 29483383).
Studies in diabetic models underpin TXL’s microvascular protective effects, relevant given diabetes-associated endothelial dysfunction in ischemic heart disease (PMID: 29912977). Furthermore, TXL improves coronary flow grade and myocardial perfusion post-PCI, promoting better left ventricular ejection fraction recovery (PMID: 27323611).
Limitations and Gaps in Current Evidence
Despite promising data, many earlier trials had small sample sizes, single-center designs, or lacked detailed baseline characterization, limiting generalizability (PMID: 31093877). Adverse events were rarely significant but gastrointestinal symptoms were more frequent with TXL in large trials (PMID: 37874574). Long-term safety data remain scarce.
Patient subgroup analyses are limited beyond genetic polymorphisms related to drug metabolism. Trials including patients with thrombolysis or endovascular therapies for stroke have not been conducted comprehensively (PMID: 39325453). Mechanistic pathways require further elucidation to translate into biomarker-guided therapy.
Expert Commentary
The reviewed literature supports Tongxinluo as a valuable complementary therapy in cardiovascular diseases characterized by ischemia and reperfusion injury, given its multi-targeted mechanism involving endothelial protection, anti-inflammatory effects, and platelet function modulation. Importantly, its efficacy synergizes with standard therapies such as PCI and dual antiplatelet therapy, offering incremental reductions in infarct size and major adverse events.
The CTS-AMI trial, with its rigorous design and large sample, provides compelling evidence for clinical benefit in STEMI. Equally, the stroke RCT indicates a potential neuroprotective role. However, heterogeneity in study designs, dosages, and endpoints across trials complicates direct comparison.
The mechanistic insights, from endothelial barrier preservation to modulation of exosomal miRNAs, not only explain TXL’s efficacy but point toward novel therapeutic targets. The enhanced benefit in genetic subgroups with clopidogrel resistance suggests personalized medicine opportunities.
Real-world applicability requires confirmation of long-term safety, standardized formulation, and further exploration in diverse ethnic and clinical settings. High-quality, multi-center RCTs incorporating advanced imaging, biomarker stratification, and longer follow-up are essential to establish TXL’s definitive therapeutic role.
Conclusion
Tongxinluo exhibits multi-faceted cardioprotective mechanisms addressing key pathophysiological processes in myocardial infarction, acute coronary syndrome, and ischemic stroke. Robust clinical evidence, notably from the CTS-AMI trial, supports its adjunctive use to reduce adverse cardiovascular events and improve functional outcomes.
Nonetheless, gaps remain in safety profiling, mechanistic understanding across disease stages, and comprehensive patient subgroup analyses. Future research priorities include:
- Large-scale, multicenter RCTs with diverse populations and standardized TXL preparations.
- Integration of biomarker-driven patient selection and mechanistic biomonitoring.
- Exploration of TXL in combination with reperfusion strategies and novel therapies like stem cell transplantation.
- Pharmacovigilance studies elucidating safety and rare adverse events.
Advancing these areas will aid incorporation of Tongxinluo into evidence-based cardiovascular therapeutic paradigms.
References
- Li S et al. Exploring the Complementary Role of Traditional Chinese Medicine in Enhancing Percutaneous Coronary Intervention Outcomes. Ther Clin Risk Manag. 2025;21:1069-1083. PMID:40666694.
- Wang Y et al. Tongxinluo and Functional Outcomes Among Patients With Acute Ischemic Stroke: A Randomized Clinical Trial. JAMA Netw Open. 2024;7(9):e2433463. PMID:39325453.
- Chen J et al. Traditional Chinese Medicine Compound (Tongxinluo) and Clinical Outcomes of Patients With Acute Myocardial Infarction: The CTS-AMI Randomized Clinical Trial. JAMA. 2023;330(16):1534-1545. PMID:37874574.
- Luo Y et al. To Investigate the Clinical Efficacy and Potential Mechanism of Tongxinluo Capsules in Preventing Coronary Restenosis. Evid Based Complement Alternat Med. 2023;2023:7985459. PMID:36743461.
- Jiang X et al. Tongxinluo-pretreated mesenchymal stem cells facilitate cardiac repair via exosomal transfer of miR-146a-5p targeting IRAK1/NF-κB p65 pathway. Stem Cell Res Ther. 2022;13(1):289. PMID:35799283.
- Li J et al. A Multicenter, Randomized, Double-Blind, and Placebo-Controlled Study of the Effects of Tongxinluo Capsules in ACS Patients with High On-Treatment Platelet Reactivity. Chin Med J (Engl). 2018;131(5):508-515. PMID:29483383.
- Yuan P et al. Tongxinluo attenuates reperfusion injury in diabetic hearts via Angptl4-mediated endothelial protection through PPAR-α pathway. PLoS One. 2018;13(6):e0198403. PMID:29912977.
- Zhang Q et al. No-reflow protection and long-term efficacy for acute myocardial infarction with Tongxinluo: ENLEAT Trial. Chin Med J (Engl). 2010;123(20):2858-64. PMID:21034597.
- Yang Y et al. Pretreatment with Tongxinluo protects porcine myocardium from ischaemia/reperfusion injury via nitric oxide mechanism. Chin Med J (Engl). 2009;122(13):1529-38. PMID:19719943.