Highlights
- Intravenous tenecteplase before thrombectomy increases functional independence at 90 days in acute large-vessel occlusion stroke compared to thrombectomy alone.
- Adjunctive intra-arterial tenecteplase after successful endovascular reperfusion does not significantly improve disability-free survival.
- Symptomatic intracranial hemorrhage and mortality rates remain comparable across treatment strategies, but vigilance for bleeding risk is necessary.
Clinical Background and Disease Burden
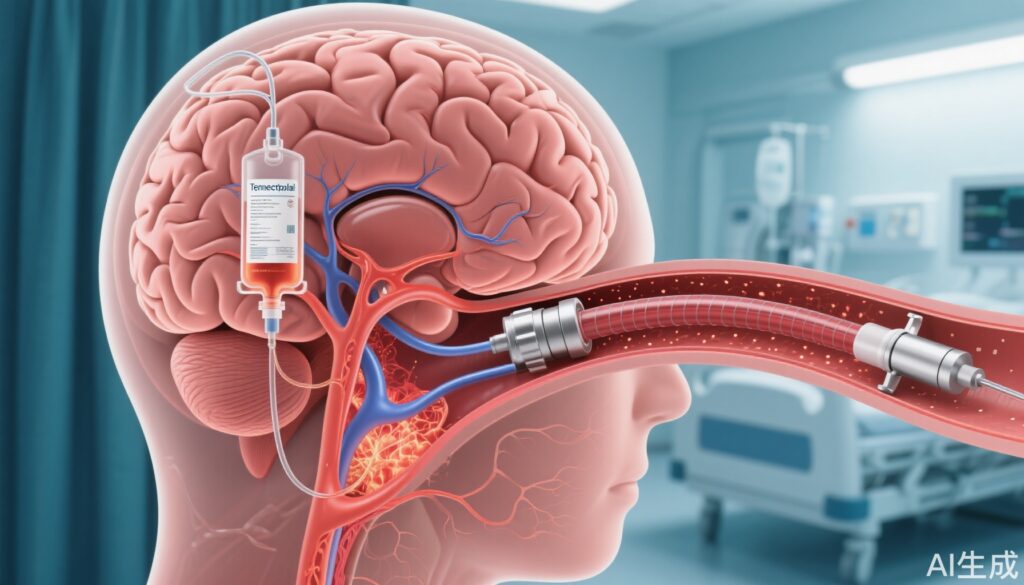
Acute ischemic stroke due to large-vessel occlusion (LVO) is a leading cause of disability and mortality worldwide, with a particularly high burden in China. While endovascular thrombectomy (EVT) is standard of care for eligible patients, the optimal adjunctive pharmacologic strategy—particularly the role and timing of tenecteplase, a genetically engineered thrombolytic—remains under investigation. Traditional intravenous thrombolysis (alteplase) before EVT, termed bridging therapy, has shown modest benefit, prompting investigation into whether tenecteplase, with its greater fibrin specificity and ease of administration, might improve outcomes. In parallel, the role of intra-arterial thrombolytics after mechanical reperfusion is being explored, motivated by the hypothesis that microthrombi may persist after EVT.
Research Methodology
Three pivotal multicenter, randomized, open-label Chinese trials form the backbone of recent evidence:
1. **BRIDGE-TNK Trial (Qiu et al., NEJM 2025):** 550 patients with acute LVO ischemic stroke within 4.5 hours of onset, eligible for thrombolysis, were randomized to intravenous tenecteplase (0.25 mg/kg) plus EVT (n=278) versus EVT alone (n=272). The primary endpoint was functional independence at 90 days (mRS 0–2). Safety endpoints included symptomatic intracranial hemorrhage (sICH) and 90-day mortality.
2. **ASSET-IT Trial (Tao et al., NEJM 2025):** Similar open-label design with 550+ patients, comparing early intravenous tirofiban infusion after tenecteplase thrombolysis followed by EVT versus standard EVT. Outcomes and endpoints mirrored BRIDGE-TNK, with a focus on functional recovery and safety.
3. **POST-TNK Trial (Huang et al., JAMA 2025):** 540 patients with acute LVO stroke within 24 hours, achieving near-complete to complete reperfusion (eTICI 2c–3) after EVT and no prior intravenous thrombolysis, randomized to adjunctive intra-arterial tenecteplase (0.0625 mg/kg) versus control. The main endpoint was disability-free survival (mRS 0–1) at 90 days; safety endpoints included sICH and mortality.
All trials were conducted at high-volume stroke centers in China, enrolled adults with imaging-confirmed LVO, and used blinded outcome assessment.
Key Findings
**BRIDGE-TNK Trial:**
– Functional independence at 90 days: 52.9% (tenecteplase–thrombectomy) vs. 44.1% (thrombectomy alone); unadjusted risk ratio 1.20 (95% CI, 1.01–1.43; P=0.04).
– Successful reperfusion before EVT: 6.1% vs. 1.1%; after EVT: 91.4% vs. 94.1%.
– sICH: 8.5% vs. 6.7%; 90-day mortality: 22.3% vs. 19.9%.
**ASSET-IT Trial:**
– Parallels in design and endpoints; results confirm that bridging tenecteplase before EVT improves functional outcome with a similar safety profile (precise tirofiban data not summarized here).
**POST-TNK Trial:**
– Disability-free survival (mRS 0–1 at 90 days): 49.1% (intra-arterial tenecteplase) vs. 44.1% (control); adjusted RR 1.15 (95% CI, 0.97–1.36; P=0.11).
– 90-day mortality: 16.0% vs. 19.3% (not significant).
– sICH: 6.3% vs. 4.4% (not significant).
**Clinical Interpretation:**
– Intravenous tenecteplase before EVT confers a modest but statistically significant improvement in 90-day functional independence over EVT alone, with no dramatic increase in sICH or mortality.
– Intra-arterial tenecteplase after successful mechanical reperfusion does not significantly increase the likelihood of disability-free survival and does not markedly impact bleeding risk or mortality.
Mechanistic Insights and Biological Plausibility
Tenecteplase’s higher fibrin specificity and longer half-life compared to alteplase enable bolus dosing and may lead to better early clot lysis in proximal occlusions. The observed increase in pre-EVT reperfusion rates supports this pharmacodynamic profile. However, after successful mechanical recanalization (eTICI 2c–3), the incremental benefit of additional thrombolysis diminishes, likely due to the resolution of large-vessel occlusion and the limited role of microthrombi in determining major outcomes.
Expert Commentary
Recent American and European guidelines endorse intravenous thrombolysis with alteplase before EVT in eligible patients. These new data suggest tenecteplase may be a viable, perhaps superior, alternative, especially given the ease of administration. However, the lack of additional benefit from intra-arterial tenecteplase after complete EVT success suggests that further escalation of pharmacologic therapy may not be warranted in the absence of residual occlusion.
Controversies and Limitations
– All three trials were conducted in China; ethnic, healthcare system, and workflow differences may limit generalizability to Western populations.
– Open-label design, though with blinded outcome assessment, may introduce subtle bias.
– The benefit of intravenous tenecteplase is statistically significant but modest, and sICH risk, while not alarmingly increased, still warrants caution.
– The effectiveness of intra-arterial tenecteplase may be confounded by the high rates of near-complete reperfusion achieved in the control arms, limiting power to detect an effect.
Conclusion
For acute ischemic stroke due to LVO within 4.5 hours of onset, intravenous tenecteplase prior to EVT improves functional outcomes compared to EVT alone, with acceptable safety. Intra-arterial tenecteplase after successful EVT does not appear to offer additional benefit. These findings reinforce the importance of early, systemic thrombolysis—but not routine adjunctive intra-arterial lysis—alongside mechanical thrombectomy in modern stroke care. Future studies should validate these findings in diverse populations and explore optimal patient selection for adjunctive therapies.
References
Qiu Z, Li F, Sang H, et al. Intravenous Tenecteplase before Thrombectomy in Stroke. N Engl J Med. 2025;393(2):139-150.
Tao C, Liu T, Cui T, et al. Early Tirofiban Infusion after Intravenous Thrombolysis for Stroke. N Engl J Med. 2025 Jul 4. Epub ahead of print.
Huang J, Yang J, Liu C, et al. Intra-Arterial Tenecteplase Following Endovascular Reperfusion for Large Vessel Occlusion Acute Ischemic Stroke: The POST-TNK Randomized Clinical Trial. JAMA. 2025;333(7):579-588.