Background and Disease Burden
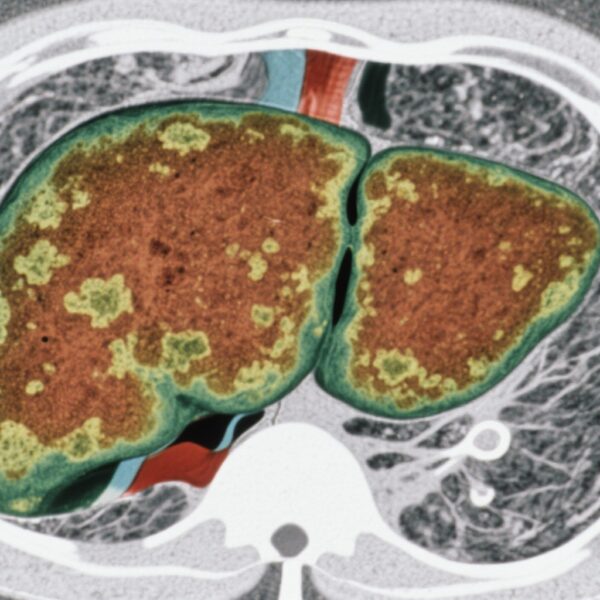
Biliary tract cancer (BTC) encompasses a heterogeneous group of malignancies arising from the biliary epithelium, including intrahepatic and extrahepatic cholangiocarcinomas as well as gallbladder cancer. Despite relatively low incidence compared to other gastrointestinal cancers, BTC carries a poor prognosis, with most patients presenting at an advanced stage where curative treatment options are limited. Median overall survival (OS) in advanced BTC remains dismal despite systemic therapies, highlighting an urgent need for effective treatments.
In clinical oncology research, overall survival has historically been considered the gold standard endpoint for evaluating therapeutic efficacy. However, OS measurement requires long follow-up durations, is influenced by post-progression therapies, and demands large sample sizes and significant resources. To expedite drug development, surrogate endpoints such as progression-free survival (PFS), objective response rate (ORR), and disease control rate (DCR) have increasingly been used in BTC trials. Surrogate endpoints can shorten trial duration and reduce costs but must reliably predict OS benefits to be clinically meaningful.
Given the heterogeneous nature of BTC and emerging novel therapeutics including immunotherapies and targeted agents, robust validation of candidate surrogate endpoints at both trial and patient levels is critical. Misleading reliance on surrogate markers could result in premature drug approvals without real survival benefit, creating potential harm and resource misallocation.
Study Design
Castet et al. performed a systematic review and meta-analysis registered under PROSPERO (CRD42023398279), encompassing 41 published phase II and III clinical trials involving 7,817 patients with advanced BTC, to evaluate correlations between candidate surrogate endpoints (PFS, ORR, DCR) and OS at the trial level. Weighted linear regression was employed to quantify associations.
Complementing this, a patient-level analysis was conducted including 2,506 individuals from five randomized clinical trials and three real-world cohorts. Patient populations spanned first-line and second-line treatment settings, with treatment modalities including chemotherapy alone and chemoimmunotherapy (e.g., chemotherapy plus durvalumab). Correlation coefficients were calculated to assess the strength of association between surrogate endpoints and OS on an individual basis. A responder analysis investigated whether radiologic response (based on standard criteria) reliably predicted survival outcomes.
Key Findings
Trial-Level Analysis
The trial-level correlation between PFS and OS was moderately strong, with an R² of 0.71 (95% CI 0.56–0.86). This indicates that approximately 71% of the variability in OS outcomes across trials could be explained by differences in PFS. In contrast, ORR demonstrated an almost negligible correlation (R² = 0.01; 95% CI 0–0.08) with OS, suggesting that radiologic tumor shrinkage rate does not reliably predict survival benefit in this population. DCR had an intermediate but modest correlation with OS (R² = 0.39; 95% CI 0.14–0.64), reflecting disease stabilization combined with responses.
Subgroup analyses by geographic region, line of therapy, and treatment modality showed consistent patterns, reinforcing the robustness of these findings across diverse clinical contexts.
Patient-Level Analysis
At the individual patient level, the correlation coefficient between PFS and OS ranged from 0.73 to 0.86 across datasets, confirming a moderate to strong association. This correlation held both for randomized trial populations and routine clinical practice cohorts, and across first- and second-line regimens.
Conversely, the responder analysis found no statistically meaningful association between achieving an objective tumor response (as defined radiologically) and improved OS. This further questions the utility of ORR as a surrogate for survival outcome.
Clinical and Regulatory Implications
The moderate correlation of PFS with OS suggests that while PFS is currently the best available surrogate endpoint for advanced BTC, it is an imperfect predictor of ultimate survival benefit. The weak correlations seen for ORR and DCR challenge their frequent use as primary endpoints, particularly for regulatory approval decisions.
These findings underscore the necessity for developing and validating novel surrogate endpoints—potentially incorporating biomarkers, functional imaging, or composite end points—that better capture meaningful clinical benefit and improved survival.
Expert Commentary
Expert oncologists emphasize that the complexity of BTC biology and the advent of immunotherapies and precision treatments necessitate reappraisal of traditional endpoints. As Dr. Juan Valle, a study co-author and leading BTC expert, notes, “Our results provide an evidence base to guide trialists and regulators but also highlight important gaps where better biomarkers and endpoints are needed to accelerate clinical advances.” This study aligns with recommendations from major oncology societies advocating for rigorous surrogate endpoint validation through meta-analytic data.
Limitations include variability in trial designs and follow-up durations, and heterogeneity in treatment regimens. However, consistency across multiple datasets strengthens the conclusions.
Conclusion
In advanced biliary tract cancer, progression-free survival shows a moderate and clinically meaningful correlation with overall survival at both trial- and patient-level analyses, supporting its use as the most reliable current surrogate endpoint. Objective response rate and disease control rate demonstrate poor to modest correlation and should be interpreted cautiously as predictors of survival benefit.
This comprehensive analysis informs clinicians, researchers, and regulatory agencies about the relative merits of common surrogate endpoints, aiding interpretation of contemporary clinical trials and facilitating informed design of future studies. Continued efforts are needed to develop surrogate endpoints with improved predictive accuracy to optimize trial efficiency and patient outcomes in this challenging disease.
Funding and Registration
This meta-analysis and patient-level evaluation were supported by multiple collaborative groups including the Spanish Cooperative Group for the Treatment of Digestive Tumors (TTD) and the DURVABTC Group. The study protocol is registered with PROSPERO under CRD42023398279.
References
Castet F, Fabregat-Franco C, Bridgewater J, et al. Association of candidate surrogate endpoints with overall survival in advanced biliary tract cancer. J Hepatol. 2025 Nov;83(5):1102-1115. doi:10.1016/j.jhep.2025.05.020.