Background
Infective endocarditis (IE) is a severe infection of the heart valves, often necessitating surgical intervention. Surgery aims to eradicate the infection, repair or replace damaged valves, and prevent complications such as heart failure or systemic embolism. However, despite established guideline recommendations indicating surgery for a substantial proportion of patients, not all eligible individuals undergo surgical treatment. Prior cohort studies typically represent select populations from tertiary referral centers, which may bias understanding of surgery utilization and outcomes. This nationwide Danish study sought to evaluate the real-world practice of surgical treatment for left-sided IE, focusing on surgery use according to established indications and associated mortality outcomes.
Study Design and Methods
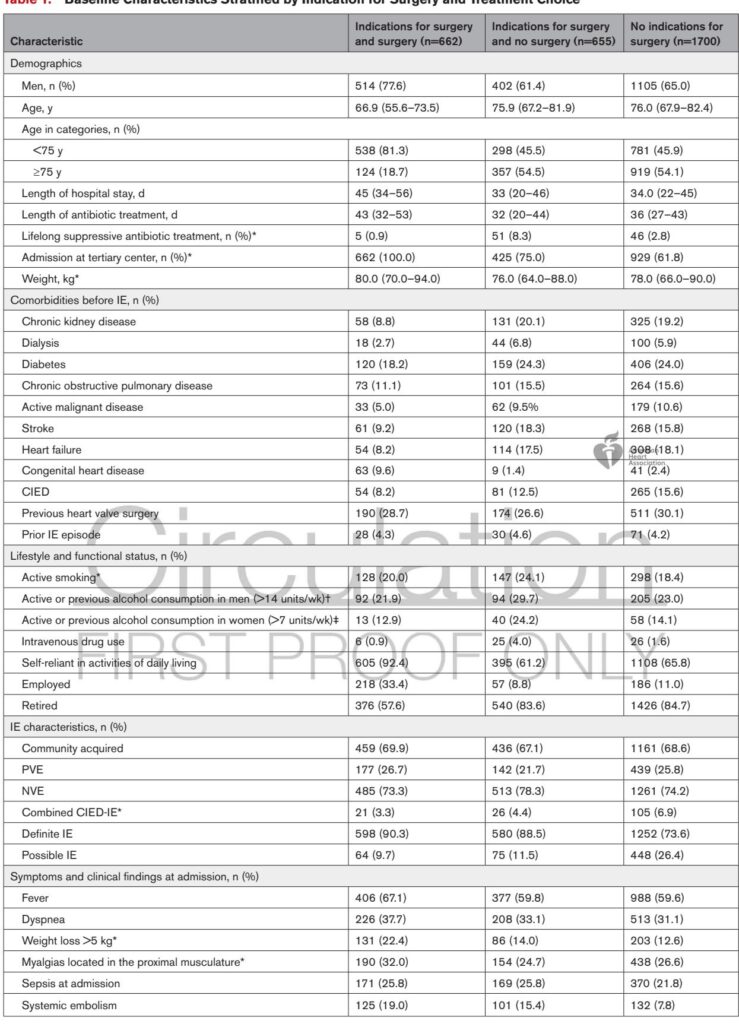
This observational cohort study utilized data from the National Danish Endocarditis Studies (NIDUS) Registry, encompassing all possible and definite left-sided IE cases in Denmark from 2016 to 2021. Patients were grouped based on surgical indications, defined as either a Class I indication per the 2015 European Society of Cardiology (ESC) guidelines or presence of vegetations ≥10 mm on diagnostic echocardiography, and on whether surgery was performed.
Data collection included detailed clinical parameters, microbiology, imaging findings, surgical timing and indications, and documented reasons for withholding surgery. Mortality was assessed at in-hospital and one-year intervals. Survival analyses used the 1-Kaplan-Meier estimator and time-dependent multivariable Cox regression models adjusted for age, sex, valve type, microbiological etiology, and relevant comorbidities. Sensitivity analyses addressed potential biases including immortal time bias and unmeasured surgical risk factors.
Key Findings
Among 3017 patients with left-sided IE, 1317 (43.7%) had absolute surgical indications. Of these, only 662 (50.3%) underwent surgery, while 655 (49.7%) received conservative medical therapy despite indications. A larger group of 1700 patients (56.5%) had no surgical indications and did not undergo surgery.
Surgically treated patients were younger (median 66.9 years) compared to those with surgical indications but untreated (median 75.9 years) and those without indications (median 76.0 years). They also had fewer comorbidities and were more likely to have Streptococcus spp infections. Conversely, patients with surgical indications who did not undergo surgery had a higher prevalence of Staphylococcus aureus infection and greater comorbidity burden, including diabetes, chronic kidney disease, and functional dependency.
In-hospital mortality was significantly higher in patients with surgical indications who did not undergo surgery (31.8%) compared to those undergoing surgery (12.5%) or those without indications (15.7%). This mortality difference persisted at one year, with rates of 50.5%, 17.0%, and 33.5%, respectively (all P5 days after diagnosis), 40.5% urgent (2-5 days), and 19.5% emergency (within 24 hours). The predominant documented reason for withholding surgery despite indication was high surgical risk or frailty, accounting for approximately 22.8% of cases where surgery was deferred.
An important finding was the underutilization of surgery in patients with large vegetations (≥10 mm), where only about one-third to half underwent surgery depending on vegetation size. Notably, more than half of the cases without surgery lacked clear documented justification, particularly for vegetation-based indications.
Expert Commentary
This comprehensive nationwide study offers valuable insights into surgical practices for left-sided IE outside of referral center bias. The data corroborate prior observations that a substantial proportion of patients with guideline-based surgical indications do not undergo surgery, often due to advanced age, comorbidities, or infections with aggressive organisms such as Staphylococcus aureus.
Notably, surgical patients had markedly better survival, consistent with accumulated evidence suggesting surgery improves outcomes in appropriate candidates. However, the younger age and lower comorbidity of surgical patients indicate confounding by indication. This bias challenges causal inference regarding surgery efficacy but underscores the clinical challenge of managing high-risk patients.
These findings reinforce the need for refined risk stratification tools integrating clinical, microbiological, and imaging data to better identify patients who may benefit from surgery despite perceived elevated operative risk. Integration of frailty assessments and enhanced perioperative care might expand surgical candidacy. Additionally, the frequent absence of documented reasons for withholding surgery highlights a potential area for quality improvement in clinical documentation and decision-making transparency.
Limitations inherent to observational registries include residual confounding and information bias, particularly regarding surgical risk metrics—which were not captured comprehensively—and incomplete documentation of withholding reasons. Randomized trials or advanced causal inference studies are warranted to inform best management strategies for high-risk patients.
Conclusion
In this nationwide Danish cohort of left-sided infective endocarditis, 40% had established indications for surgery, but only half underwent surgical treatment. Surgical patients had substantially better survival yet were significantly younger with fewer comorbidities and less frequent Staphylococcus aureus infection. High surgical risk remains the predominant reason for conservative management despite indications. These findings highlight the critical need to balance surgical benefits against operative risks and to enhance decision-making frameworks, particularly for high-risk patients. Further prospective and interventional studies are essential to optimize management strategies and improve outcomes for this complex population.
References
Graversen PL, Østergaard L, Hadji-Turdeghal K, Møller JE, Bruun NE, Povlsen JA, Moser C, Smerup M, Søgaard P, Jensen HS, Modrau IS, Jensen AD, Petersen JK, Havers-Borgersen E, Stahl A, Helweg-Larsen J, Faurholt-Jepsen D, Bundgaard H, Iversen K, Køber L, Fosbøl EL. Clinical Practice of Surgical Treatment for Left-Sided Infective Endocarditis: Nationwide Data from the NIDUS Registry. Circulation. 2025 Aug 21. doi: 10.1161/CIRCULATIONAHA.125.074608. Epub ahead of print. PMID: 40836922.