Highlight
- Starting treatment with surgery yields a significantly higher recovery rate at 18 months compared to corticosteroid injection in carpal tunnel syndrome patients.
- Recovery was defined by a validated six-item carpal tunnel syndrome scale, with 61% recovery in the surgery group versus 45% in the injection group.
- Adverse event rates were similar between groups, with only one serious complication requiring hospitalization in the surgery group and no treatment-related deaths reported.
- The trial supports surgical intervention as a first-line treatment option for sustained carpal tunnel syndrome relief.
Study Background and Disease Burden
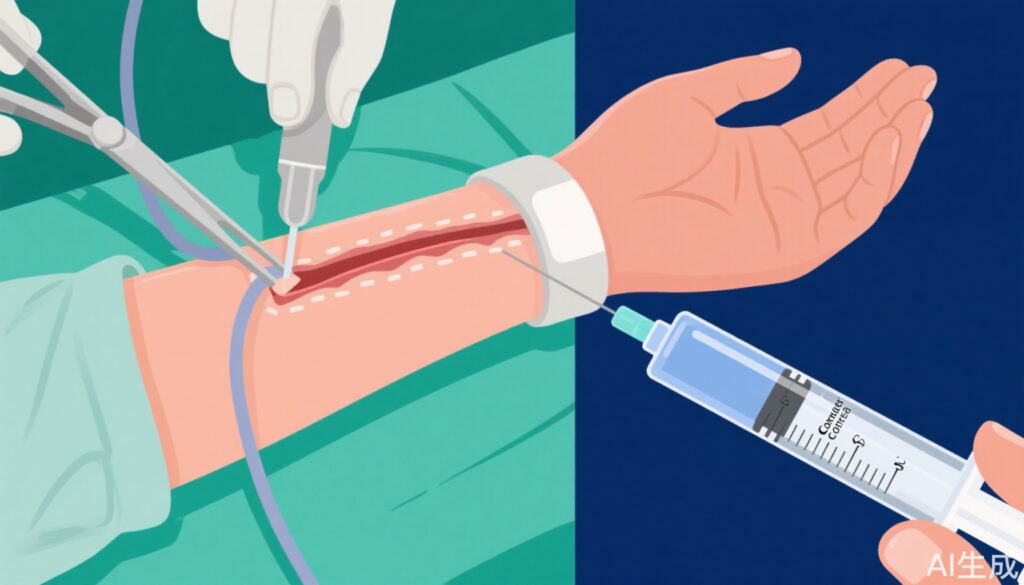
Carpal tunnel syndrome (CTS) is one of the most common entrapment neuropathies, characterized by compression of the median nerve at the wrist. It manifests clinically with numbness, tingling, and pain in the hand, which can lead to functional impairment and reduced quality of life. Treatment options include conservative management, corticosteroid injections, and surgical decompression. While corticosteroid injections provide temporary relief, surgery is considered the definitive treatment. However, the optimal initial treatment strategy remains debated, especially regarding long-term outcomes and safety. The DISTRICTS trial was designed to address this clinical uncertainty by comparing initial surgical treatment to initial corticosteroid injection in patients with confirmed CTS.
Study Design
This was an open-label, multicentre, randomised controlled trial conducted across 31 hospitals in the Netherlands. Eligible participants were adults diagnosed with CTS for at least six weeks, confirmed by electrophysiological or sonographic testing. A total of 934 patients (545 female, 389 male) were randomized 1:1 to start either with surgery (n=468) or a corticosteroid injection (n=466).
Randomisation was stratified based on symptom laterality (unilateral vs bilateral), presence of concomitant diseases as risk factors, and history of previous ipsilateral injections. The interventions allowed additional treatments if needed, such as further injections or surgery, reflecting real-world clinical practice. The primary outcome was the proportion of patients who achieved recovery at 18 months, defined by a score less than eight points on the six-item CTS symptom scale, analyzed in the intention-to-treat population.
Key Findings
At 18 months, data were available for 805 participants (86%). Recovery rates were significantly higher in the surgery group: 61% (243/401) compared to 45% (180/404) in the injection group, with a relative risk of 1.36 (95% CI 1.19–1.56, p<0.0001). This indicates a 36% increased chance of recovery when surgery is the initial treatment.
Adverse events occurred in 86% of surgery patients and 85% of injection patients, reflecting the common occurrence of minor side effects in both groups. Only one serious adverse event requiring hospitalization occurred in the surgery group. No treatment-related deaths were reported, underscoring the overall safety of both interventions.
The allowance for additional treatments after initial allocation reflects a pragmatic approach, yet the superiority of surgery as initial treatment remained clear. This suggests that early surgical decompression may prevent prolonged nerve compression, leading to better functional outcomes.
Expert Commentary
The DISTRICTS trial provides robust, high-quality evidence favoring surgery as the first-line intervention for patients with confirmed carpal tunnel syndrome. The long-term follow-up of 18 months strengthens the clinical applicability of these findings, addressing limitations of earlier studies that often had shorter durations.
Some experts note that while injections may offer temporary symptom relief and are less invasive, the durability of benefit is limited. Surgery, although involving operative risks, provides more sustained symptom resolution. The similar adverse event rates reinforce that surgery is generally safe when performed by experienced clinicians.
Limitations include the open-label design, which could influence patient-reported outcomes. However, objective electrophysiological or sonographic confirmation at baseline and standardized outcome measures mitigate bias. The generalizability is supported by the multicentre nature and broad inclusion criteria, though applicability to patients with mild or atypical CTS remains to be confirmed.
Conclusion
In patients with carpal tunnel syndrome of at least six weeks’ duration confirmed by diagnostic testing, initiating treatment with surgical decompression results in significantly higher recovery rates at 18 months compared to starting with corticosteroid injection. Despite similar adverse event profiles, surgery offers a more durable clinical benefit. These findings support consideration of early surgery as the preferred initial treatment strategy in appropriate patients, potentially improving long-term outcomes and reducing the need for subsequent interventions.
References
Palmbergen WAC, Beekman R, Heeren AM, van Nuenen BFL, Alleman TWH, Verstraete E, Jellema K, Verhagen WIM, Visser LH, de Ruiter GCW, van de Beek D, de Borgie CAJM, Bogaards JA, de Bie RMA, Verhamme C; Dutch CTS study group. Surgery versus corticosteroid injection for carpal tunnel syndrome (DISTRICTS): an open-label, multicentre, randomised controlled trial. Lancet. 2025 Jun 14;405(10495):2153-2163. doi: 10.1016/S0140-6736(25)00368-X. PMID: 40517008.