Highlight
– Preoperative stereotactic radiation therapy (SRT) shows similar safety to postoperative SRT in treating brain metastases.
– Preoperative SRT significantly shortens the treatment timeline, accelerating time to completion.
– No significant differences in 30-day postoperative morbidity or postprocedural events between pre- and postoperative SRT.
– Higher completion rates of both treatments observed in the preoperative SRT arm compared to postoperative.
Study Background and Disease Burden
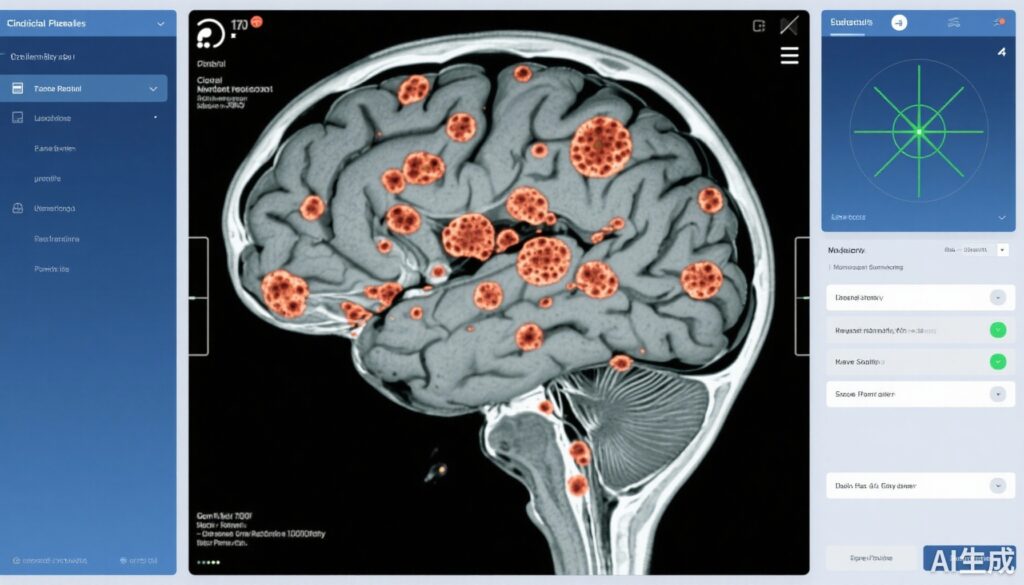
Brain metastases represent a substantial clinical challenge in oncology, occurring in approximately 20-40% of adult cancer patients during their disease course. These lesions significantly impact neurological function, quality of life, and overall survival. Standard treatment approaches often combine surgical resection and stereotactic radiation therapy (SRT) to maximize local control while preserving neurological function. Conventionally, SRT is administered postoperatively; however, this sequence may delay adjuvant treatment due to surgical recovery and present logistical challenges. Additionally, the timing of radiation in relation to surgery could influence toxicity profiles and treatment efficacy. Thus, assessing the feasibility, safety, and logistical advantage of administering SRT preoperatively presents an opportunity to potentially optimize multidisciplinary brain metastases management.
Study Design
This single-institution phase 3 randomized clinical trial enrolled 103 patients aged 18 years or older with brain metastases, who were candidates for planned surgical resection and stereotactic radiation therapy. Key inclusion criteria included an Eastern Cooperative Oncology Group (ECOG) Performance Status of 2 or better and eligibility for SRT within 30 days of surgery. Patients with radiosensitive tumor histologies (such as small cell lung cancer or lymphoma), unknown primary brain metastasis, or radiographic leptomeningeal disease were excluded.
Participants were randomized 1:1 into two cohorts: the preoperative SRT group received 1 to 5 fractions of SRT followed by surgical resection within one month of radiation. The postoperative SRT group underwent surgical resection first, followed by SRT within one month post-surgery. The primary and secondary endpoints focused on the safety profile, feasibility, postprocedural morbidity, radiation management logistics, and toxic effect outcomes.
Key Findings
The study population comprised 103 patients with a median age of 59 years (range 26-83), including 54.4% males. Among them, 83 patients (80.6%) completed both radiation and surgical treatments during the study. At enrollment, most patients (84%) presented with 1 to 4 brain metastases, while 13% had 5 to 10 lesions, and 2% had more than 10.
Completion rates were higher in the preoperative SRT cohort, with 88% completing both treatments, compared to 73% in the postoperative cohort. Importantly, there were no statistically significant differences in 30-day postoperative morbidity or postprocedural adverse events between the two groups, underscoring comparable safety profiles.
A notable logistical advantage was observed with preoperative SRT: the median interval between surgery and SRT was significantly shorter at 6 days (range 0-24) versus 22 days (range 12-42) in the postoperative cohort (P < .001). Moreover, the overall median duration from randomization to completion of both brain-directed therapies was 10 days (range 4-31) in the preoperative arm compared with 32.5 days (range 19-55) in the postoperative arm (P < .001). This accelerated timeline may translate into earlier adjuvant treatment initiation, potentially improving oncological outcomes and patient convenience.
Additionally, the study reported comparable radiation therapy management practices, indicating that preoperative SRT is feasible within existing clinical workflows.
Expert Commentary
This randomized study provides critical evidence supporting the clinical utility of preoperative SRT for patients undergoing surgery for brain metastases. The comparable safety profile and reduced treatment duration address key clinical barriers in multidisciplinary oncologic care. Preoperative radiation may also confer theoretical biological advantages, such as sterilization of microscopic tumor margins before surgical manipulation and reduced tumor cell dissemination risk.
However, the findings should be contextualized within the study’s constraints, notably being a single-institution trial with a relatively limited sample size and nonprimary endpoint focus on safety and logistics. Further multicenter studies with longer follow-up are warranted to assess long-term oncologic outcomes, including local control, neurocognitive effects, and overall survival.
Guidelines for managing brain metastases have increasingly recognized stereotactic approaches, but the optimal timing relative to surgery remains under investigation. This trial contributes valuable prospective clinical data that may influence evolving standards and patient-centered care pathways.
Conclusion
In summary, this phase 3 randomized clinical trial demonstrates that preoperative stereotactic radiation therapy for brain metastases is as safe as postoperative administration, with significant benefits in shortening the time to treatment completion. These findings suggest that preoperative SRT is a feasible and efficient alternative that may improve treatment logistics and facilitate expedited multidisciplinary management. Future research should aim to corroborate these results in larger cohorts and assess long-term oncological and neurocognitive outcomes to better define the role of preoperative SRT in clinical practice.
References
- Yeboa DN et al. Therapy, Safety, and Logistics of Preoperative vs Postoperative Stereotactic Radiation Therapy: A Preliminary Analysis of a Randomized Clinical Trial. JAMA Oncol. 2025 Aug 1;11(8):890-899. doi: 10.1001/jamaoncol.2025.1770.
- Margolin K, Linskey ME. Management of brain metastases: an overview. Compr Physiol. 2017 Jan;7(1):663-695. doi: 10.1002/cphy.c160006.
- Yang TJ, Wu AJ, Henke LE. Impact of radiation therapy timing on outcomes in patients with brain metastases undergoing surgical resection. Neurosurg Focus. 2020 Aug;49(2):E13. doi: 10.3171/2019.11.FOCUS19602.