Introduction and Context
The relationship between sleep, circadian rhythms and Alzheimer’s disease (AD) has emerged as a major focus in aging research. Sleep disturbances are common in older adults and frequently precede cognitive decline and overt dementia. A growing body of observational and mechanistic work suggests a bidirectional relationship: neurodegenerative changes disturb sleep and circadian systems, and disturbed sleep may in turn accelerate pathophysiologic processes linked to AD. Yet progress has been hampered by highly variable methods across studies—different questionnaires, differing durations and processing of actigraphy, mixed use of polysomnography (PSG) and emerging wearables—making synthesis difficult and slowing translation.
To address this, the Sleep and Circadian Rhythms Professional Interest Area of the International Society to Advance Alzheimer’s Research and Treatment (ISTAART) convened international experts and used a modified Delphi process to produce research-focused consensus recommendations. The findings appear in André et al., “International recommendations for sleep and circadian research in aging and Alzheimer’s disease: A Delphi consensus study” (Alzheimers Dement. 2025) and set a pragmatic, research-oriented minimum standard for future work in the field [1].
Why these recommendations matter now
– Rapid growth in sleep and dementia research, plus the proliferation of consumer and research-grade wearables, make harmonized methods urgent.
– Better comparability across cohorts will strengthen inference about whether and how sleep disturbance contributes to AD risk, and whether sleep-targeted treatments can prevent or slow cognitive decline.
– These recommendations aim to improve data quality, reporting consistency and prioritization of key unanswered questions—essential steps toward clinical trials and ultimately clinical practice guidance.
New Guideline Highlights
Major recommendations and themes from the Delphi consensus (André et al.) are:
– Prefer objective measures whenever feasible: PSG/EEG for standard sleep architecture and microstructure; actigraphy for multi-night, real-world rest-activity and napping assessments.
– Define a minimum and an ideal recording duration for actigraphy: avoid <7 days; minimum standard 7–13 days; ideal ≥14 days.
– Always combine actigraphy with a sleep diary to improve interpretation and data quality.
– Avoid single-item self-report sleep questions; re-validate common questionnaires for older adults and people with cognitive impairment, or develop geriatric-specific instruments.
– Use research-quality (validated, raw-data-accessible) devices preferentially; interpret consumer-device outputs with caution until validated in older and cognitively impaired populations.
– Document a standardized minimum dataset about participants (core variables) and a core-plus set (strongly encouraged) including biomarker status and APOE ε4.
– Prioritize longitudinal designs, multi-night monitoring, mechanistic EEG analyses (spectral analyses, connectivity, slow waves and spindles) and clinical trials of sleep and circadian interventions.
Key takeaways for clinicians and researchers
– For research studies focused on aging and AD, emphasize objective, multi-night measurement and rigorous reporting of participant characteristics and medications.
– When using consumer devices, treat outputs as exploratory unless devices have peer-reviewed validation and provide raw data for analysis.
– Trials are needed to test whether treating sleep disorders meaningfully alters cognitive trajectories and AD biomarkers; the panel prioritized such trials.
Updated Recommendations and Key Changes from Prior Practice
Context: Prior to this consensus, there were growing but fragmented statements on wearable-device use and sleep metrics; however, no international, research-focused consensus existed specifically for aging and AD research.
What’s new or clarified in this consensus (compared with prior, less formal practice):
– Standardized minimum dataset (core and core-plus items) for participant characterization in sleep–AD research (Boxed below). Prior studies often reported age and sex alone; the consensus mandates additional comorbidities, medication classes and sleep-specific diagnoses.
– A clear minimum and ideal actigraphy duration (minimum 7 days, ideal ≥14 days), and strong recommendation to pair actigraphy with sleep diaries—formalizing a practice that previously varied widely.
– Explicit distinction between research-quality and consumer-quality wearable/nearable devices, with stated confidence levels for measurement validity in older and cognitively impaired populations.
– Priority ranking of sleep/circadian features for future research: circadian rhythms, obstructive sleep apnea (OSA), REM sleep metrics, EEG connectivity and spectral analyses, harmonization of actigraphy, insomnia, napping, sleep fragmentation, spindles and N3/slow-wave sleep.
– Practical electrode-site prioritization for PSG/EEG in research settings (F3, F4, C3, C4, O1, O2 highlighted) to aid harmonization of EEG data collection.
Driving evidence for the updates
– Rapid improvements and wider availability of wearable EEG, multi-sensor actigraphy and consumer trackers motivated the panel to explicitly separate device classes and recommend validation work in older adults [10,11].
– Mechanistic work on slow-wave activity, glymphatic function and amyloid dynamics (e.g., Ju et al., Mander) supports prioritizing N3/slow waves and quantitative EEG features [6,8].
– The panel prioritized longitudinal evidence and intervention trials because current observational associations (e.g., between sleep fragmentation or OSA and cognitive decline) cannot prove causation; trials are needed to test modification of risk.
Topic-by-Topic Recommendations
Below is a topic-oriented synthesis of the consensus recommendations and practical guidance for researchers.
1) Core and core-plus participant data (what to collect and report)
Core (mandatory):
– Cognitive diagnosis (normal, preclinical AD, MCI, AD dementia) and standardized cognitive measures.
– Education level.
– Body mass index (BMI).
– Key comorbidities: neurological conditions, depressive symptoms/psychiatric disorders, cardiovascular disease.
– Alcohol intake and current shift work status.
– Sleep-related diagnoses and treatments: insomnia symptoms, OSA diagnosis and OSA treatment status, restless legs syndrome.
– Medication classes: benzodiazepines, non-benzodiazepine hypnotics (Z-drugs), antidepressants, other hypnotics (e.g., dual orexin receptor antagonists, ramelteon), trazodone, antipsychotics.
Core-plus (strongly recommended if available):
– Biomarker profile (amyloid, tau, neurodegeneration markers using CSF or PET or validated plasma biomarkers).
– APOE ε4 genotype.
Rationale: These items address common confounders/modifiers of sleep and cognition, and reporting them improves comparability across studies.
2) Measurement modalities and when to use them
Polysomnography (PSG)/EEG:
– Priority for standard sleep architecture and microstructure measures (e.g., sleep stages, arousals, spectral power, slow-wave characteristics, spindles).
– Both in-lab and validated at-home PSG/EEG are acceptable in preclinical AD and MCI; for AD dementia, at-home PSG/EEG is often preferred to maximize ecological validity and tolerability.
– Recommended electrode prioritization (endorsed by >40% of the panel): F3, F4, C3, C4, O1, O2 (additional leads such as Cz, Fz, Pz as useful when feasible).
Actigraphy/accelerometry:
– Recommended for multi-night monitoring of rest–activity patterns and daytime napping.
– Minimum recommended recording: 7–13 days; ideal: ≥14 consecutive days.
– Require a concurrent sleep diary to capture sleep timing, naps, caffeine/alcohol/medication use and subjective disturbance; diaries also support quality-control and epoch selection.
– Data processing: recommend use of validated algorithms, combination of software-implemented and in-house approaches, and explicit reporting of scoring thresholds and algorithms used.
Self-report and informant report:
– Avoid reliance on single-item questions; standard validated questionnaires (e.g., PSQI, ISI) should be re-validated for older populations and cognitive impairment.
– For preclinical AD, patient self-report may be informative; for MCI and AD dementia, informant-report often provides better reliability but cognitive status of informant should be documented.
Wearables and nearables (EEG headbands, smartwatches, rings, mattress sensors):
– Distinguish research-quality devices (validated, raw-data-accessible, regulatory approvals when relevant) from consumer devices (black-box algorithms, proprietary scoring).
– Strong guidance: prioritize research-quality devices and require validation in older adults and cognitively impaired populations before using consumer-device outputs for primary endpoints.
– Combine EEG-based wearables with complementary sensors (heart rate, oximetry) whenever possible to enrich interpretation; panel endorsed home oximetry for OSA screening in cognitively unimpaired older adults.
3) Specific sleep and circadian features to measure (Box 1 from consensus)
Core objective features (actigraphy and/or PSG/EEG):
– Sleep fragmentation indices (number of awakenings, arousals, stage shifts).
– Sleep efficiency and wake after sleep onset (WASO).
– Total sleep time and sleep duration.
– Time spent in sleep stages (N1, N2, N3, REM) and stage percentages.
– NREM spectral power and slow-wave characteristics (including slow-wave activity magnitude and morphology).
– REM spectral power and REM-related EEG slowing.
– Daytime activity metrics, timing, variability, and daytime rest/napping episodes.
Core clinical/self-reported features:
– General sleep disturbance and poor sleep quality.
– Insomnia symptoms (difficulty initiating/maintaining sleep, non-restorative sleep).
– Excessive daytime sleepiness (e.g., Epworth Sleepiness Scale).
4) Actigraphy specifics: durations and diary use
– Minimum: 7 consecutive days; ideal: ≥14 days for robust circadian and variability measures.
– Always pair with a simple sleep diary probing latency, timing, naps, caffeine/alcohol/medication use, morning refreshment and night-time disruptions.
– Explicitly report the algorithm used for sleep/wake scoring, any adjustments made from diary data, and epoch length.
5) Polysomnography specifics
– Prefer PSG/EEG for studies aiming to examine sleep microarchitecture (slow waves, spindles), arousal indices, OSA severity, and other physiological signals.
– For multi-site or cohort studies, harmonize electrode montage around the recommended core sites and share processing pipelines when possible.
6) Medication and exposure reporting
– Record psychotropic and sleep medication exposures, with the panel favoring a one-month look-back window for medication use when designing clinical trials; shorter windows (2 weeks to 1 week) were also permitted but less favored.
7) Data sharing and harmonization
– The panel strongly recommended creating a global consortium for sleep and dementia data sharing and harmonization (to standardize variables, processing pipelines and to enable pooled analyses across cohorts).
Expert Commentary and Insights
Panel perspectives
– The expert panel emphasized a pragmatic balance: prioritize objective measures (PSG/EEG and actigraphy) yet recognize feasibility constraints—at-home monitoring, longer actigraphy durations and validated wearables are pragmatic ways to scale studies.
– The panel repeatedly highlighted the need for validation of devices and algorithms in older and cognitively impaired groups rather than extrapolating performance from young, healthy cohorts.
– A strong consensus emerged that single-night snapshots (one-night PSG or short actigraphy) are inadequate for many research questions; multi-night and continuous monitoring better capture variability and circadian features.
Controversies and areas without consensus
– The panel did not universally endorse replacement of full PSG by wearable EEG devices; confidence was mixed for research-quality EEG wearables and low for consumer EEG devices. Further validation studies remain essential.
– Relative roles of in-lab versus at-home PSG depend on the study question and participant group: there was no blanket preference for one or the other across all settings.
Clinical implications of the research recommendations
– Although these recommendations target research, they have immediate implications for clinical trials and eventual clinical practice. Standardized assessment will enable clearer trials of sleep interventions and clearer determination whether sleep modification can prevent or slow AD.
– Clinicians should be cautious interpreting consumer-device sleep metrics in older patients and should prioritize validated tools when sleep assessment will inform treatment decisions.
Practical Implications
For research teams planning new studies
– Include the consensus core dataset in study CRFs; report these variables in publications to facilitate pooling.
– Prefer validated actigraphs and aim for ≥7 days of recording; when possible, target ≥14 days.
– Use sleep diaries alongside actigraphy; disclose algorithms and scoring rules in methods.
– If using consumer devices, undertake a validation substudy against PSG/actigraphy or use research-quality sensors for primary endpoints.
For funders and consortium builders
– Support longitudinal, multi-site cohorts with harmonized protocols including sleep and circadian measures.
– Fund validation studies of wearables in older and cognitively impaired populations.
– Support clinical trials testing whether treatment of OSA, insomnia or circadian misalignment alters cognitive decline or AD biomarkers.
Patient vignette (illustrative)
– Mary Johnson, 66, with subjective memory complaints and fragmented sleep. A research team following the consensus would: characterize her clinically (cognitive testing, education, BMI, comorbidities), obtain 14 days of wrist actigraphy plus a sleep diary to assess fragmentation and napping, perform at-home EEG/PSG if microarchitecture is a focus, document medications/status of OSA, and—if part of a trial—measure AD biomarkers and APOE status as core-plus data.
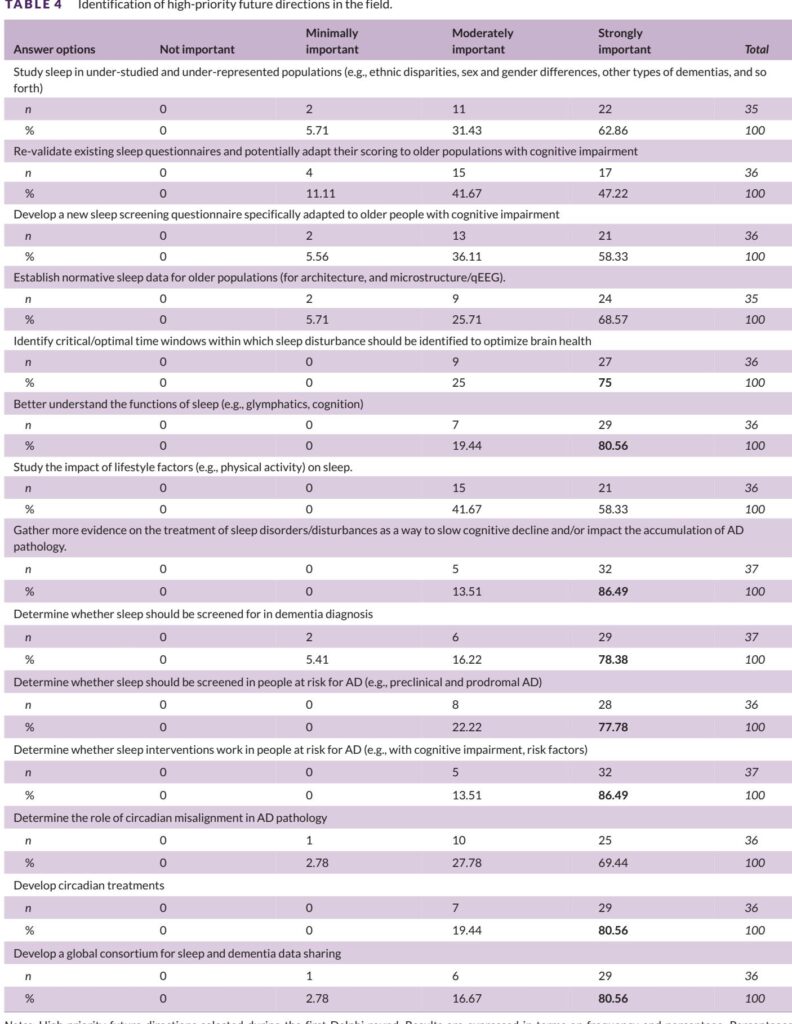
High-priority Research Agenda (Boxed Synthesis)
Top five research priorities from the consensus:
1. Longitudinal cohort studies with repeated sleep and circadian measures to define trajectories and temporality.
2. Randomized clinical trials testing whether sleep and circadian interventions (OSA therapy, insomnia treatment, circadian entrainment) affect cognition and AD biomarkers.
3. Harmonization of actigraphy methodologies and development of shared processing pipelines.
4. Validation studies of wearable and nearable devices specifically in older adults and people with MCI/AD dementia.
5. Studies of understudied populations including sex-stratified samples, people with shift-work histories, racial/ethnic minorities, non-AD dementias, and middle-aged adults (40–65 years).
References
1. André C, Stankeviciute L, Michaelian JC, et al.; Sleep and Circadian Rhythms Professional Interest Area of ISTAART. International recommendations for sleep and circadian research in aging and Alzheimer’s disease: A Delphi consensus study. Alzheimers Dement. 2025 Oct;21(10):e70742. doi:10.1002/alz.70742.
2. Livingston G, Huntley J, Liu KY, et al. Dementia prevention, intervention, and care: 2024 report of the Lancet standing Commission. Lancet. 2024;404(10452):572–628. doi:10.1016/S0140-6736(24)01296-0.
3. Ju YE, Lucey BP, Holtzman DM. Sleep and Alzheimer disease pathology–a bidirectional relationship. Nat Rev Neurol. 2014;10(2):115–119. doi:10.1038/nrneurol.2013.269.
4. Bubu OM, Brannick M, Mortimer J, et al. Sleep, cognitive impairment, and Alzheimer’s disease: a systematic review and meta-analysis. Sleep. 2017;40(1):zsw032. doi:10.1093/sleep/zsw032.
5. Mander BA. Local sleep and Alzheimer’s disease pathophysiology. Front Neurosci. 2020;14:525970. doi:10.3389/fnins.2020.525970.
6. de Zambotti M, Goldstein C, Cook J, et al. State of the science and recommendations for using wearable technology in sleep and circadian research. Sleep. 2024;47(4):zsad325. doi:10.1093/sleep/zsad325.
7. De Zambotti M, Cellini N, Goldstone A, Colrain IM, Baker FC. Wearable sleep technology in clinical and research settings. Med Sci Sports Exerc. 2019;51(7):1538–1557. doi:10.1249/MSS.0000000000001947.
8. Ong JL, Golkashani HA, Ghorbani S, et al. Selecting a sleep tracker from EEG-based, iteratively improved, low-cost multisensor, and actigraphy-only devices. Sleep Health. 2024;10(1):9–23. doi:10.1016/j.sleh.2023.11.005.
9. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4.
10. Lee T, Cho Y, Cha KS, et al. Accuracy of 11 wearable, nearable, and airable consumer sleep trackers: prospective multicenter validation study. JMIR Mhealth Uhealth. 2023;11:e50983. doi:10.2196/50983.
Notes: The references above include the primary Delphi consensus (André et al.) as well as foundational and recent literature on sleep, dementia, and wearable validation. The consensus statement is intended as research guidance and does not replace future clinical practice guidelines; the authors of the Delphi study indicated that clinical recommendations will follow in a separate publication.