Highlight
- Exercise echocardiography combined with peripheral venous pressure measurement (CPETecho-PVP) offers superior pathophysiological insight in Fontan circulation failure compared to standard cardiopulmonary exercise testing.
- The study identifies that an elevated peripheral venous pressure to cardiac output (PVP/CO) slope (>3 mm Hg/L/min) is associated with worse clinical status, including higher NYHA class and common Fontan complications.
- A steeper PVP/CO slope correlates with lower peak oxygen consumption, diminished heart rate reserve, and reduced cardiac index, indicating impaired exercise capacity.
- These findings support integrating CPETecho-PVP into routine clinical evaluation to guide management in adult Fontan patients.
Study Background and Disease Burden
The Fontan procedure provides life-saving palliation for patients with complex congenital heart defects resulting in single-ventricle physiology. Despite improved survival into adulthood, the unique Fontan circulation often faces progressive failure characterized by elevated systemic venous pressures, reduced cardiac output, and exercise intolerance. Evaluating Fontan failure remains challenging, with standard cardiopulmonary exercise testing (CPET) offering valuable but incomplete insights into hemodynamic derangements. Peripheral venous pressure measurement during exercise echocardiography (CPETecho-PVP) has been proposed to capture pressure-flow relationships unique to the Fontan circulation more directly. Understanding such parameters could facilitate better patient risk stratification and tailored interventions in this vulnerable population, which continues to incur significant morbidity and mortality related to circulatory failure and associated complications such as arrhythmias, thromboembolism, and pulmonary pathology.
Study Design
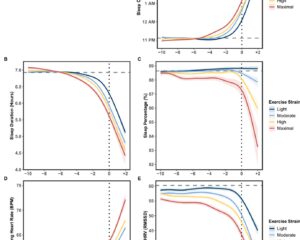
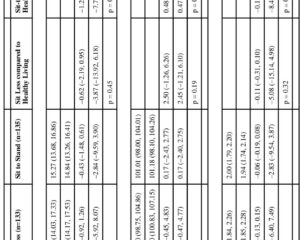
This prospective observational study enrolled 41 consecutive patients with established Fontan circulation, median age 28 years (range 17 to 60 years), predominately with left ventricular dominance (78%). Participants underwent CPETecho-PVP, wherein peripheral venous pressure (PVP) was measured via an 18- to 20-gauge intravenous catheter placed in the distal upper extremity during exercise. Simultaneously, cardiac output (CO) was derived with echocardiographic methods to construct multipoint pressure-flow plots. Linear regression of these plots generated a PVP/CO slope, with a threshold of >3 mm Hg/L/min defining elevated slope indicative of pathological response. Clinical data including NYHA functional class, pulmonary pathology, arrhythmia and thromboembolism history, and N-terminal prohormone of natriuretic peptide (NT-proBNP) levels were collected. Additional assessment included peak oxygen consumption (peak VO2), heart rate reserve, and peak cardiac index during exercise. Statistical analysis compared clinical and exercise parameters across groups with elevated versus normal slopes and evaluated determinants of exercise capacity.
Key Findings
The study demonstrated that patients with a PVP/CO slope >3 mm Hg/L/min (n=12) had significantly worse clinical profiles compared to those with slope ≤3 mm Hg/L/min (n=29). Key associations include:
– Higher prevalence of advanced NYHA class III-IV (P =.005), indicating poorer functional status.
– Greater incidence of lung pathology (P =.004), atrial arrhythmias (P =.009), and thromboembolic events (P =.02), reflecting disease complexity and Fontan-related complications.
– Elevated median NT-proBNP levels (325.0 vs. 150.5 ng/L; P =.034), a biomarker of cardiac stress and unfavorable prognosis.
– Markedly reduced exercise capacity as assessed by peak VO2 (48.7% ± 13.3% predicted vs 65.2% ± 15.3%; P =.003).
– Lower heart rate reserve (65% vs 100% predicted; P =.010) and diminished peak cardiac index (3.8 ± 0.8 L/min·m² vs 6.3 ± 1.5 L/min·m²; P <.001), indicative of impaired cardiac responsiveness and output augmentation.
Multivariate analyses implicated the PVP/CO slope, alongside rest-to-peak heart rate and cardiac index changes and pulmonary function (forced vital capacity), as independent correlates of exercise capacity measured by percent predicted peak VO2.
Expert Commentary
This study provides compelling evidence that semi-invasive pressure-flow plots obtained through CPETecho-PVP serve as an effective surrogate for Fontan hemodynamic assessment, bridging the gap between noninvasive testing and more invasive catheterization-based evaluations. The strong correlation between elevated PVP/CO slope and clinical complications underlines the slope as a potential marker for Fontan failure severity. Notably, the methodology exploits peripheral venous pressure as a proxy for systemic venous pressure unique to this population, offering novel insights during exercise when circulatory demands reveal hidden insufficiencies.
While promising, the study is limited by its modest sample size and inherent single-center design, which may affect generalizability. Additionally, the technique requires technical expertise and infrastructure for synchronized echocardiography and pressure monitoring. Future multicenter studies with longitudinal follow-up are warranted to validate prognostic value and assess impact on clinical decision-making. Integration within standard protocols could allow earlier identification of Fontan patients at risk, optimizing timing for interventions such as medical therapy escalation, catheter-based palliation, or transplantation referral.
Conclusion
Semi-invasive pressure-flow assessment integrating exercise echocardiography with peripheral venous pressure measurement (CPETecho-PVP) unveils clinically relevant hemodynamic derangements in adult Fontan patients. A steeper PVP/CO slope exceeds 3 mm Hg/L/min and correlates with deteriorated clinical status and substantially reduced exercise capacity. This approach enhances our understanding of Fontan physiology, suggesting significant translational potential for routine surveillance and individualized management. Adoption of CPETecho-PVP could refine risk stratification and therapeutic strategies in this growing patient population facing complex circulatory challenges.
References
1. Cieplucha A, Van Belle H, Miranda WR, Bekhuis Y, Decorte E, Michielsen M, De Meester P, Troost E, Cattapan I, Rosseel T, Verwerft J, Claessen G, Cornelissen VA, Goetschalckx K, Gewillig M, Budts W, Van De Bruaene A. Semi-invasive pressure-flow plots obtained using exercise echocardiography relate to clinical status and exercise capacity in patients with a Fontan circulation. J Am Soc Echocardiogr. 2025 Sep;38(9):843-854. doi:10.1016/j.echo.2025.05.007.
2. Ghai A, Goldman JH, Doucette S, et al. Comprehensive clinical assessment of adult Fontan patients and relationship to outcomes. Congenit Heart Dis. 2018;13(5):825-832.
3. d’Udekem Y, Iyengar AJ, Galati JC, et al. Redefining expectations of long-term survival after the Fontan procedure: twenty-five years of follow-up from the entire population of Australia and New Zealand. Circulation. 2014;130(11 Suppl 1):S32-S38.
4. Khairy P, Radojevic J, Lakshminrusimha S, et al. Assessment of prognostic variables in adult Fontan patients using echocardiographic and cardiopulmonary exercise testing. Int J Cardiol. 2012;161(3):178-183.
5. Rosenthal DN, Landzberg MJ. Clinical outcomes of adult Fontan patients: a call for better diagnostic and therapeutic strategies. Heart. 2016;102(8):553-555.