Study Background and Disease Burden
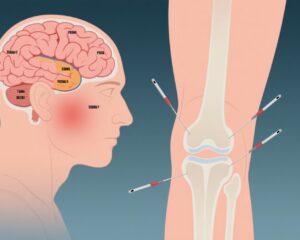
Chronic fatigue syndrome (CFS), also known as myalgic encephalomyelitis, is a debilitating disorder characterized by persistent, unexplained fatigue that significantly reduces quality of life. Despite extensive research, effective medical therapies remain limited, leaving many patients with unmet treatment needs. Among the multifactorial pathophysiological hypotheses, autonomic nervous system (ANS) dysfunction is recognized as a pivotal contributor to symptom persistence in CFS. Heart rate variability (HRV) is a noninvasive marker reflecting the balance between sympathetic and parasympathetic nervous system activity and has been increasingly used to assess autonomic regulation in CFS patients. Traditional Chinese medicine interventions such as acupuncture and moxibustion have been employed to restore autonomic balance and improve symptoms, though robust clinical evidence on their physiological mechanisms and comparative efficacy remains sparse. This study by Li et al. (2025) directly addresses these gaps by evaluating the effects of different acupuncture techniques and moxibustion on HRV and fatigue symptoms in patients with CFS.
Study Design
This randomized controlled clinical trial enrolled 175 patients diagnosed with CFS and 35 healthy controls. The patients were randomly assigned to five intervention groups (35 patients per group): fake acupuncture (Group B), acupuncture at bilateral Zusanli (ST36) points (Group C), acupuncture at Guanyuan (CV4) point (Group D), combined acupuncture at both ST36 and CV4 (Group E), and moxibustion at both ST36 and CV4 points (Group F). A healthy control group (Group A) was included for baseline comparisons.
Fake acupuncture involved superficial needling without penetration or stimulation at the relevant acupoints to serve as a placebo control. Treatments were administered every other day, totaling 10 sessions for each group. Symptom assessments included the Qi-deficiency Syndrome Score, CFS Score, and SF36 Health Survey Score prior to treatment. HRV parameters were measured at baseline, after the first treatment, after the fourth treatment, and at treatment completion to evaluate both immediate and cumulative autonomic effects.
Key Findings
The study found that both acupuncture and moxibustion significantly alleviated fatigue symptoms compared to fake acupuncture, with the combination of acupuncture and moxibustion being the most effective. HRV analysis revealed nuanced differences in autonomic modulation by the different interventions:
1. Immediate HRV Effects: Acupuncture predominantly influenced rapid changes in HRV parameters indicating enhanced parasympathetic tone and reduced sympathetic activity after single sessions, suggesting quick autonomic adjustments.
2. Long-term HRV Regulation: Moxibustion exhibited superior efficacy in sustaining improvements in HRV measures after the full treatment course, reflecting durable autonomic rebalancing.
3. Acupoint-Specific Effects: Targeting both the Zusanli (ST36) and Guanyuan (CV4) points simultaneously generated greater symptom improvement and more comprehensive modulation of both sympathetic and parasympathetic branches than single-point stimulation.
4. Mechanistic Insights: The Zusanli (ST36) point likely modulates parasympathetic pathways, while the Guanyuan (CV4) point appears to influence sympathetic regulation. Their combined stimulation synergistically enhances overall autonomic balance.
Across all measures, combined acupuncture and moxibustion treatment yielded the greatest clinical and physiological benefits, underscoring the complementary mechanisms of these traditional therapies.
Expert Commentary
These findings contribute significantly to the clinical validation of acupuncture and moxibustion in managing CFS, particularly through modulation of the autonomic nervous system. The trial’s rigorous design, including placebo controls and objective HRV endpoints, strengthens the evidence base beyond purely subjective symptom reports.
However, the study is limited by its relatively small sample size per group and the short duration of follow-up, making it unclear how durable treatment effects may be over months or years. Future research should investigate long-term outcomes, dose-response relationships, and potential biochemical mediators to further elucidate the mechanisms underlying these interventions.
The distinct regulatory roles of acupoints ST36 and CV4 in autonomic function also warrant exploration in other autonomic disorders beyond CFS. Integration of these findings with current neuroimmunological models of fatigue may guide multimodal therapeutic strategies.
Conclusion
This randomized controlled trial demonstrates that acupuncture and moxibustion are effective therapies for alleviating fatigue symptoms in CFS patients by regulating heart rate variability and autonomic nervous system function. Acupuncture shows more immediate improvements in autonomic tone, while moxibustion offers more sustained benefits. The combination of both, particularly targeting the Zusanli (ST36) and Guanyuan (CV4) points, optimizes treatment outcomes through complementary modulation of parasympathetic and sympathetic nervous systems. These results provide a strong rationale for incorporating targeted acupuncture and moxibustion into integrative management approaches for CFS and warrant further studies on their long-term clinical impact.
References
Li T, Litscher G, Zhou Y, Song Y, Shu Q, Chen L, Huang Q, Wang Y, Tian H, Teng R, Wang H, Liang F. Effects of acupuncture and moxibustion on heart rate variability in chronic fatigue syndrome patients: Regulating the autonomic nervous system in a clinical randomized controlled trial. Complement Ther Med. 2025 Sep;92:103184. doi: 10.1016/j.ctim.2025.103184. Epub 2025 Apr 30. PMID: 40315935.
Trial registration: Approved by the Medical Ethics Committee of Hubei Provincial Hospital of Traditional Chinese Medicine (Approval number: HBZY2016-C24-01), and registered with the North American Clinical Trials Data Center (ClinicalTrials.gov) (05/10/2016) (registration number: NCT02924831).