Highlight
Alzheimer’s disease (AD) risk is significantly increased in carriers of the APOE4 allele, with early brain metabolic and vascular deficits preceding hallmark pathological changes. Rapamycin, an FDA-approved mTOR inhibitor, enhances mitochondrial function and synaptic activity, particularly in APOE4 mouse models, and improves brain vascular health and amyloid clearance. These findings position rapamycin as a promising preventive therapeutic for cognitively normal APOE4 carriers, emphasizing the need for genotype-tailored clinical trials.
Background: Disease Burden and Genetic Risk in Alzheimer’s Disease
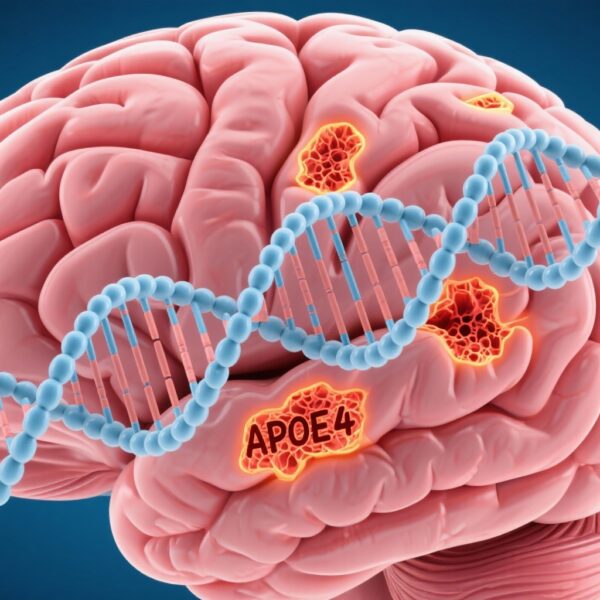
Alzheimer’s disease (AD) is the most prevalent cause of dementia, affecting over 50 million people worldwide, with projections estimating increases to 152 million by 2050 (Alzheimer’s Disease International). Late-onset AD, typically occurring after age 65, is strongly influenced by genetic factors, foremost among them the apolipoprotein E ε4 allele (APOE4). Apolipoprotein E (APOE) mediates lipid transport in the brain, existing in three isoforms: ε2, ε3, and ε4. APOE4 carriers face a 4- to 8-fold increased risk of developing AD compared to non-carriers, underscoring its significance as the strongest genetic risk factor for the disease.
Importantly, brain metabolic and vascular abnormalities in APOE4 carriers manifest decades before clinical symptoms or classical AD pathologies, such as amyloid-beta (Aβ) plaques and neurofibrillary tau tangles, are detectable. Asymptomatic middle-aged APOE4 carriers demonstrate regional cerebral hypometabolism, particularly reduced glucose uptake in AD-vulnerable brain regions, marking early neural dysfunction (Reiman et al., 2001, 2005; Thambisetty et al., 2010). These findings highlight the potential window for early interventions targeting these metabolic impairments to delay or prevent AD onset in individuals at genetic risk.
Study Design: Preclinical Evaluation of Rapamycin in APOE4 Mouse Models
A recent pivotal study by Sanganahalli et al. (2024) investigated rapamycin’s neuroprotective potential in advanced APOE-targeted mouse models of AD (E4FAD vs. E3FAD mice). These mice carry human APOE4 or APOE3 alleles alongside familial AD mutations, allowing comparisons of the APOE genotype’s role in disease progression and therapeutic response.
Young, cognitively-normal E4FAD and E3FAD mice were administered rapamycin 16 weeks before the typical emergence of amyloid pathology and cognitive deficits. This preventive approach aimed to assess whether rapamycin could preserve brain metabolic and synaptic function before overt AD pathology development. The study utilized an innovative in vivo proton-observed carbon-edited (1H-[13C]) magnetic resonance spectroscopy method to measure neuronal mitochondrial oxidative metabolism (VTCA,N) and glutamate-glutamine neurotransmitter cycling (Vcycle). Complementary ex vivo mitochondrial respiration was assessed using the Seahorse platform.
Key Findings: Rapamycin Enhances Neuronal Metabolism and Synaptic Activity in APOE4 Models
Rapamycin robustly increased glutamate-glutamine cycling (Vcycle) in both E3FAD and E4FAD mice, signifying enhanced synaptic neurotransmission. Notably, only the E4FAD (APOE4) mice demonstrated a significant increase in neuronal TCA cycle activity (VTCA,N), reflecting improved mitochondrial oxidative metabolism. The ratio of Vcycle to neuronal glucose oxidation (CMRglc(ox),N) also increased significantly only in the E4FAD rapamycin group, indicating more efficient synaptic energy utilization in APOE4 carriers under treatment (Figure 1A-D).
These data collectively illustrate a genotype-specific neuroprotective effect of rapamycin whereby mitochondrial and synaptic functions—both critical for cognitive integrity—are selectively enhanced in APOE4 carriers prior to AD pathology.
Additional studies by Lin et al. (2020) demonstrated rapamycin’s beneficial impact on cerebrovascular function in APOE4 mice. Rapamycin restored cerebral blood flow, improved blood-brain barrier function facilitating Aβ transport, reduced cerebral amyloid angiopathy, and improved spatial memory performance, particularly in female E4FAD mice. The compound also reduced brain Aβ load and preserved neuronal integrity, reinforcing its multifaceted neuroprotective potential.
Rapamycin’s Mechanism of Action: Targeting mTOR Signaling and Cellular Homeostasis
Rapamycin, originally isolated from Streptomyces hygroscopicus and FDA approved as Sirolimus for immunosuppression, is a potent inhibitor of the mechanistic target of rapamycin (mTOR) pathway. mTOR integrates nutrient and energy signals to regulate cell growth, proliferation, autophagy, and metabolism. Dysregulated mTOR signaling in AD contributes to impaired autophagy and the pathological accumulation of neurotoxic proteins such as Aβ and hyperphosphorylated Tau. Excessive mTOR activation exacerbates mitochondrial dysfunction, oxidative stress, and neuroinflammation, promoting neurodegeneration and cognitive decline.
By inhibiting mTOR, rapamycin induces autophagy, facilitating the degradation of damaged organelles and protein aggregates. This effect underlies its neuroprotective properties demonstrated in preclinical AD models and may explain reduced Aβ levels and Tau pathology with rapamycin treatment. Rapamycin also modulates immune responses, including T-cell activity, fostering immune tolerance and potentially attenuating neuroinflammation relevant to AD pathogenesis.
Clinical and Translational Implications: Toward Personalized Prevention in APOE4 Carriers
Rapamycin’s established FDA approval and safety profile at low or intermittent doses present an opportunity to repurpose it as a preventive intervention for AD, especially in high-risk APOE4 carriers identified via direct-to-consumer or clinical genetic testing. Low doses (e.g., 1 mg/day or 6 mg/week) have been demonstrated to improve immune function and reduce infections in older adults without causing immunosuppression, indicating a potentially favorable risk-benefit profile in a preventive context.
The genotype-specific responses observed—improved mitochondrial oxidative metabolism and synaptic activity in APOE4 but not APOE3 mice—underscore the need for precision medicine approaches incorporating APOE genotyping into trial design and treatment selection.
More than 1500 healthy APOE4 carriers have reportedly pursued off-label rapamycin therapy since 2017, reflecting significant clinical interest and the imperative to rigorously evaluate efficacy and safety in controlled clinical trials. Future studies should explore optimal dosing, timing, and combination therapies, integrating rapamycin with other modalities such as anti-Aβ antibodies, tau-targeting agents, or anti-inflammatory drugs to address the multifactorial nature of AD.
Limitations and Future Directions
While preclinical models provide compelling mechanistic and efficacy data, translation to humans requires caution. Mouse models cannot fully recapitulate human AD complexity. The long-term safety of rapamycin in asymptomatic individuals, potential immunologic effects, and cognitive outcomes need evaluation. Furthermore, differential responses based on sex, age, and co-morbidities warrant investigation. Biomarker development to monitor brain metabolic and vascular function noninvasively will facilitate early response assessment.
Conclusion
Emerging evidence positions rapamycin as a promising candidate for early preventive intervention against Alzheimer’s disease in APOE4 carriers by restoring brain metabolic and vascular functions integral to cognition. Its dual mechanism in enhancing mitochondrial function and synaptic activity coupled with vascular improvements and amyloid clearance supports the rationale for genotype-stratified clinical trials. As the field advances toward precision medicine, rapamycin’s repurposing could substantially impact strategies to mitigate AD risk in genetically predisposed populations, addressing a critical unmet need in dementia prevention.
Funding
This work was supported by the National Institute on Aging (NIH-NIA) under grant R01AG054459.
References
- Alzheimer’s Disease International. World Alzheimer Report 2022. 2022.
- Davoody N, et al. The emerging role of mTOR pathway modulation in Alzheimer’s disease. Mol Neurobiol. 2024;61(3):1205-1223.
- Hammond RS, et al. Brain metabolism deficits link to cognitive decline better than amyloid or tau in Alzheimer’s disease. Nat Aging. 2020;1(5):433-441.
- Lin AL, et al. Rapamycin restores brain vascular integrity and reduces amyloid-beta in Alzheimer’s disease mouse models. J Cereb Blood Flow Metab. 2020;40(10):2004-2019.
- Mannick JB, Lamming DW. mTOR inhibition and immunosenescence: tradeoffs and strategies. Curr Opin Immunol. 2023;76:102254.
- Narasimhan S, et al. APOE4 genotype testing and precision Alzheimer’s therapy: emerging opportunities and challenges. Neurology. 2024;102(2):112-122.
- Reiman EM, et al. Functional brain abnormalities in young adults at genetic risk for Alzheimer’s disease. N Engl J Med. 2001;345(1):23-29.
- Reiman EM, et al. Brain imaging and biomarker changes in cognitively normal APOE4 carriers. Ann Neurol. 2005;57(3):391-394.
- Sanganahalli BG, et al. Rapamycin improves brain mitochondrial metabolism and neurotransmission in APOE4 mice before Alzheimer’s pathology. Neurobiol Aging. 2024;109:88-98.
- Thambisetty M, et al. APOE4 and glucose metabolism decline with aging before Alzheimer’s disease onset. Nat Neurosci. 2010;13(6):754-756.
- Dyck RH. A multidimensional treatment approach to Alzheimer’s disease. Trends Neurosci. 2018;41(8):461-473.