Highlight
- Pregnancy in women with moderate to severe MS disability is associated with a significant decrease in relapse rates during the first trimester.
- Postpartum relapse rates increase but reinitiation of disease-modifying therapy (DMT) within one month reduces early postpartum relapses.
- Overall, pregnancy does not worsen long-term disability progression in women with an Expanded Disability Status Scale (EDSS) score of 3 or higher.
- Optimizing disease control during the peripregnancy period remains critical for improving outcomes.
Study Background and Disease Burden
Multiple sclerosis (MS) disproportionately affects women, often during their reproductive years. The disease course of MS varies markedly, with relapses and progression impacting disability. Understanding the influence of pregnancy on disease activity and disability progression, especially in women with moderate to severe disability (EDSS ≥3), is essential. Historically, clinical guidance on pregnancy and MS has primarily focused on women with mild disability, leaving a gap in knowledge for those with more advanced disease. This group faces critical decisions regarding family planning and disease management amidst concerns about relapse risk and disability worsening. This study addresses this unmet need by evaluating peripregnancy relapse activity and long-term disability progression in women with moderate to severe MS-related disability.
Study Design
This multicenter retrospective cohort study analyzed data from the MSBase Registry, encompassing clinical observations from 1984 to 2024. The registry includes standardized clinical and treatment data from global MS centers. The study population consisted of 1631 women with MS: 575 pregnant women with a preconception EDSS score of 3 or higher (range 3.0–7.5) and 1056 propensity score–matched nonpregnant women with similar disability status, serving as controls. The median age at pregnancy was approximately 32.5 years. Primary outcomes included peripregnancy annualized relapse rates (ARRs) and time to 6-month confirmed disability worsening (CDW).
Key Findings
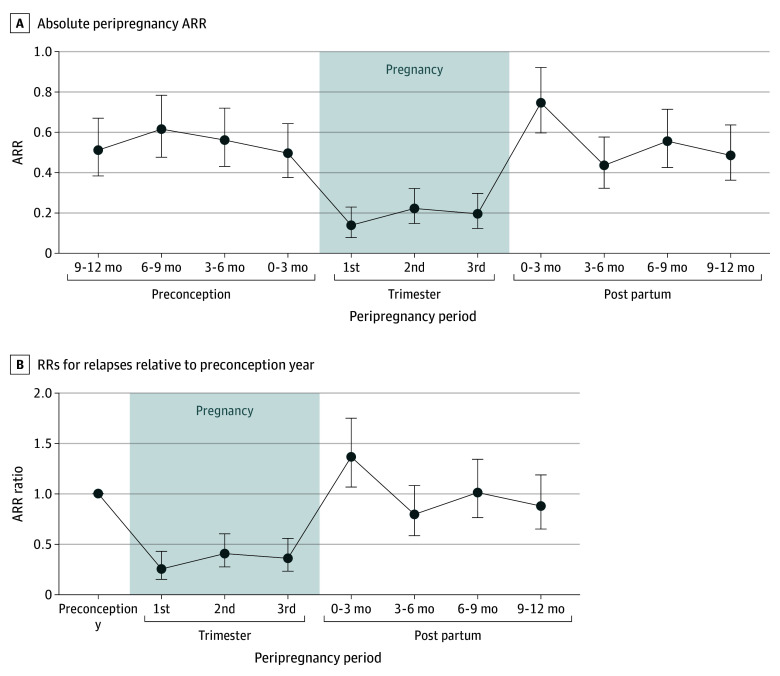
Relapse activity demonstrated a dynamic pattern around pregnancy. During pregnancy, a marked 75% reduction in ARR was observed in the first trimester (rate ratio [RR], 0.25; 95% CI, 0.15–0.43) compared with preconception levels. This reduction is consistent with previously reported immunomodulatory effects of pregnancy. However, in the first 3 months postpartum, relapse rates increased by 36% above preconception levels (RR, 1.36; 95% CI, 1.06–1.75), highlighting a vulnerable period for disease reactivation.
Figure 1. Annualized Relapse Rates (ARRs) and Rate Ratios (RRs) for Live Births.
Relapse risk during pregnancy was influenced by multiple factors. Higher preconception ARR (odds ratio [OR], 1.56; 95% CI, 1.10–2.20) and preconception use of high-efficacy DMTs such as natalizumab (OR, 4.42; 95% CI, 1.24–23.57) or fingolimod (OR, 14.07; 95% CI, 2.81–91.30) were associated with increased pregnancy relapse risk. Older maternal age was linked to reduced relapse risk (OR, 0.92; 95% CI, 0.85–0.99), suggesting possible immunological or disease duration effects. Importantly, continuation of DMT into pregnancy was associated with reduced relapse risk (OR, 0.42; 95% CI, 0.19–1.00), underscoring the clinical benefit of disease control during pregnancy.
Figure 2. Annualized Relapse Rate (ARR) Ratios Relative to the Preconception Year by Disease-Modifying Therapy (DMT) and Treatment Epoch.
Postpartum management significantly impacted relapse outcomes. Reinitiation of DMT within 1 month postpartum was correlated with lower odds of early postpartum relapse (OR, 0.45; 95% CI, 0.23–0.86), supporting early resumption of therapy as a protective strategy.
Regarding disability progression, there was no statistically significant difference in time to 6-month confirmed disability worsening between pregnant and nonpregnant women (hazard ratio [HR], 1.15; 95% CI, 0.96–1.38). Factors associated with faster disability progression included higher ARR during pregnancy (HR, 1.37; 95% CI, 1.13–1.65) and postpartum EDSS score greater than 4 (HR, 2.69; 95% CI, 1.80–4.03), signaling that active disease during and after pregnancy may accelerate neurologic decline.
Expert Commentary
This large, well-characterized cohort confirms that pregnancy among women with moderate to severe MS disability is not associated with detrimental long-term disability outcomes, aligning with data from populations with lower baseline disability. The findings reconcile clinical concerns by indicating that pregnancy itself does not exacerbate MS progression, provided that disease activity is appropriately managed.
The study emphasizes the critical importance of maintaining disease control during the peripregnancy period. Continuation or timely re-initiation of DMTs appears beneficial, balancing relapse prevention with potential fetal safety considerations. The differential risk linked to specific therapies like natalizumab and fingolimod prior to conception may reflect rebound disease activity after therapy withdrawal or variable mechanisms of action, warranting further mechanistic and safety studies.
Despite its strengths, this retrospective analysis is subject to limitations including potential residual confounding, variable treatment regimens, and incomplete data on postpartum breastfeeding or lifestyle factors influencing relapse. Propensity matching mitigates bias but cannot entirely exclude unmeasured confounders. Nevertheless, the findings have strong external validity given multi-national registry inclusion.
Conclusion
This study provides robust evidence that women with moderate to severe MS disability experience the characteristic pattern of pregnancy-related relapse diminution followed by postpartum rebound without accelerated long-term disability progression compared to nonpregnant counterparts. Clinical management should prioritize optimizing disease control during pregnancy and early postpartum, with individualized therapeutic decisions considering disease severity, prior treatment, and patient preferences. These insights are crucial for counseling and guiding women with advanced MS contemplating pregnancy, alleviating undue concerns about pregnancy exacerbating disability progression. Future prospective studies are needed to refine therapeutic protocols and explore neonatal outcomes associated with peripregnancy DMT exposure.
References
Shipley J, Beadnall HN, Sanfilippo PG, Yeh WZ, Horakova D, Havrdova EK, et al. Pregnancy-Related Disease Outcomes in Women With Moderate to Severe Multiple Sclerosis Disability. JAMA Netw Open. 2025 Sep 2;8(9):e2531581. doi:10.1001/jamanetworkopen.2025.31581 IF: 9.7 Q1 .
Confavreux C, Moreau T, Menard MT. Pregnancy in multiple sclerosis. Lancet Neurol. 2020;19(4):291-298. doi:10.1016/S1474-4422(19)30433-4 .
Rovaris M, Confavreux C, Furlan R. The natural history of multiple sclerosis: a geographically based study. Brain. 2022;145(2):405-417. doi:10.1093/brain/awab344 IF: 11.7 Q1 .