Current psychiatric diagnostic systems, including the Diagnostic and Statistical Manual of Mental Disorders (DSM) and the International Classification of Diseases (ICD), offer valuable frameworks that facilitate clinical communication, research, prescribing, and healthcare organization. However, these systems primarily rely on symptom-based categories that exhibit significant heterogeneity and overlapping features across disorders, indicating limited biological validity. Mental disorders originate from complex brain biology interacting bidirectionally with environmental factors, but this knowledge is not reflected in current classification schemas. Diagnosis heavily depends on qualitative assessments and subjective patient reports, leading to potential overdiagnosis or underdiagnosis and contributing to heterogeneous patient populations in clinical trials. These limitations hinder the development and approval of effective, mechanism-based treatments.
Contemporary advances in neuroscience, high-throughput technologies, computational methods, and digital phenotyping enable more precise, quantitative characterization of mental disorders incorporating biological, behavioral, and environmental dimensions. Digital tools, for example, can provide continuous objective monitoring of behavioral changes. Importantly, environmental influence—termed the exposome—and its interaction with biological processes are crucial in shaping psychiatric phenotypes. Against this backdrop, the European College of Neuropsychopharmacology (ECNP) has initiated a global Precision Psychiatry Roadmap (PPR) to transition from traditional symptom-based frameworks toward a biologically informed, dynamic diagnostic system facilitating precise patient stratification and mechanism-driven treatment.
Development and Methodology of the Precision Psychiatry Roadmap
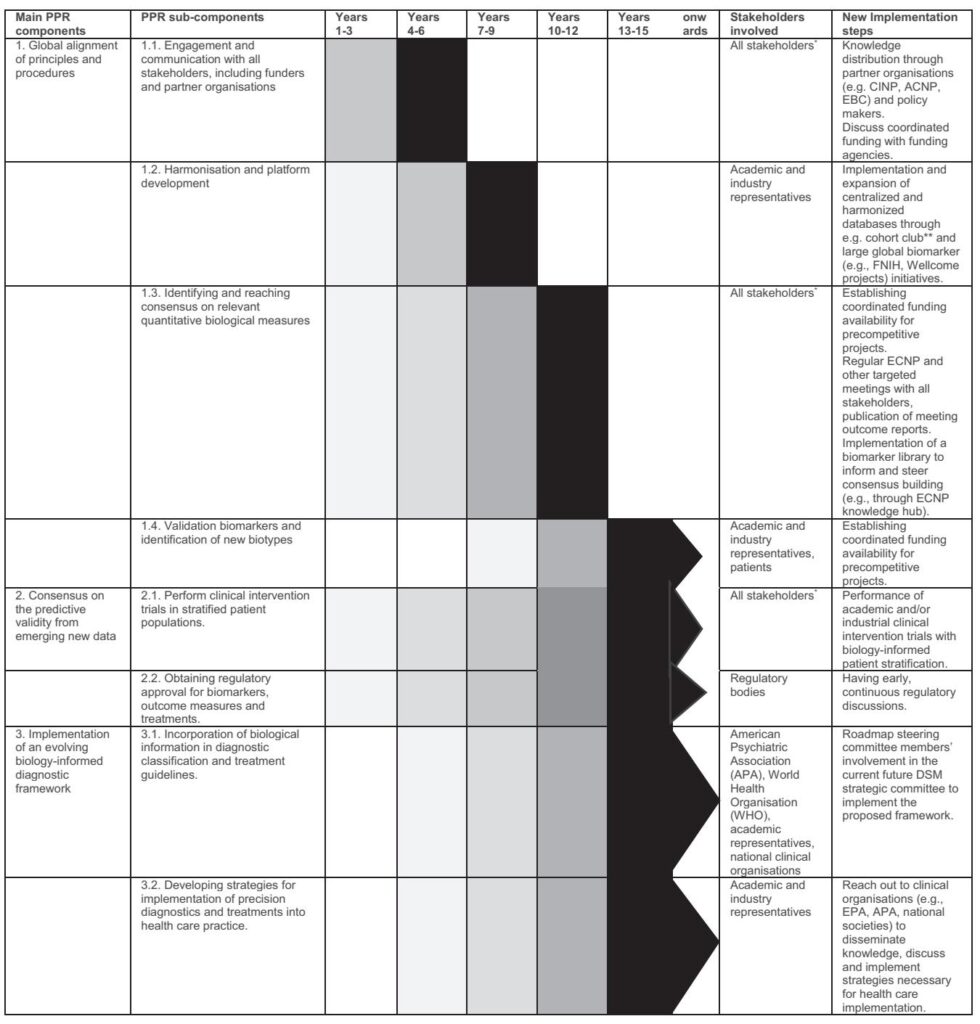
Following the 2024 ECNP New Frontiers Meeting, a multidisciplinary steering committee comprising academia, industry, regulatory agencies, and patient advocacy groups convened to define and implement the PPR. The process involved iterative discussions through in-person and virtual meetings to establish guiding principles, strategic goals, and timelines. A writing group translated stakeholder feedback into a comprehensive roadmap aiming at global harmonization of research methodologies and clinical paradigms. The PPR emphasizes coordinated multi-stakeholder collaboration and data sharing to continuously integrate emerging biological evidence into psychiatric nosology.
Implementation Strategy of the Precision Psychiatry Roadmap
The PPR comprises three primary domains:
- Global Alignment: Achieving consensus among scientists, clinicians, industry, regulators, payers, patients, and policymakers worldwide to harmonize principles, procedures, and goals. This ensures incorporation of sociocultural, ethnic, and socioeconomic factors affecting mental health into the framework.
- Consensus Building on Predictive Validity: Validating emerging biological, behavioral, and environmental biomarkers through rigorous, large-scale studies and replicable clinical trials to stratify patient subgroups accurately and predict treatment response.
- Operationalizing Biology-Informed Frameworks: Iteratively updating diagnostic classifications and treatment guidelines based on accumulating evidence, supported by educational initiatives to facilitate clinical adoption.
Harmonizing assessment tools and methodologies across diagnostic categories is a critical initial step. Current fragmentation in symptom measurement and biomarker research impairs cross-disorder comparisons. Projects like the Psychiatric Genomics Consortium and the ENIGMA consortium exemplify large-scale, harmonized efforts in genomics and neuroimaging that have advanced understanding.
Population-based cohorts such as UK Biobank and the ABCD study, complemented by well-characterized patient-based longitudinal cohorts (e.g., the Accelerating Medicines Partnership for Schizophrenia), provide rich datasets to uncover biological underpinnings and treatment predictors. Multi-site, large clinical trials with stringent methodological rigor are essential to translate biomarker discoveries into clinically actionable tools. Barriers such as privacy regulations and heterogeneous data collection require international standardization and innovative analytic solutions (e.g., federated learning) to enable data sharing.
Biomarkers and Biology-Driven Hypotheses in Precision Psychiatry
Validated biomarkers are indispensable for a biology-informed psychiatric framework and precision therapeutics. Biomarkers can be diagnostic, prognostic, predictive, pharmacodynamic, or related to safety and risk. Diverse modalities including neuroimaging, genetic/omics, physiological, biofluid, and digital measures will likely contribute in multimodal combinations, reflecting the complex biological processes underlying psychiatric disorders.
The success of biomarker-driven diagnosis in Alzheimer’s disease, exemplified by the amyloid/tau/neurodegeneration (ATN) framework and FDA approval of targeted therapies, provides a paradigm for psychiatry. Analogous transdiagnostic biological constructs—such as reward circuitry dysfunction in anhedonia or threat processing alterations in PTSD—are being elucidated through circuit-based models. These models inform clinical trial designs targeting circuit dysfunction transcending traditional diagnostic boundaries.
There is notable progress in linking molecular, cellular, circuit, behavioral, and environmental data to generate mechanistic hypotheses. For instance, NMDA receptor autoantibodies in psychosis or genetic syndromes like Fragile X associated with autism spectrum symptoms highlight rare causal biology, whereas common disorders involve many biological pathways requiring multimodal data integration.
Integration of mechanism-based nomenclature for pharmacotherapies, reflecting targets and biological pathways rather than broad categories like “antidepressants,” is anticipated to facilitate precision treatment development and guide therapeutic use.
Validation, Clinical Application, and Evolution of the Diagnostic Framework
Robust biomarker validation involves analytical validation, internal clinical validation, and external validation to ensure reproducibility, predictive validity, and generalizability. Overfitting and small datasets currently limit most candidate biomarkers. Establishing minimal standards and employing large, harmonized cohorts are critical to advance biomarker qualification for regulatory approval.
Clinical stratification by biologically informed subtypes is necessary for successful therapeutic trials and regulatory endorsement. The road to integration includes iterative refinement through clinical research, regulatory dialogue, and stakeholder engagement. Concurrently, clinical practice guidelines and educational programs must evolve to incorporate biology-informed diagnostics and treatments.
Recognizing the importance of developmental, environmental, sex, and resilience factors, population-based longitudinal studies can elucidate risk trajectories, critical exposure windows, and protective mechanisms to inform prevention strategies.
Conclusion
The Precision Psychiatry Roadmap delineates a visionary, evidence-driven path toward transforming psychiatric nosology by incorporating biological and behavioral measures alongside symptomatic assessment. While acknowledging the ambitious and long-term nature of this endeavor, gradual implementation with defined milestones involving global multi-stakeholder collaboration offers promise for more precise diagnosis, personalized treatment, and ultimately reduced burden from mental disorders. Support from funding agencies, regulatory bodies, and the healthcare ecosystem is essential to accelerate this transition. Continued research integrating neurobiology, environment, and digital phenotyping will refine understanding and operationalize precision psychiatry in clinical practice.
Reference
Kas MJH, Penninx BWJH, Knudsen GM, Cuthbert B, Falkai P, Sachs GS, Ressler KJ, Bałkowiec-Iskra E, Butlen-Ducuing F, Leboyer M, Marston H, Luthman J, Mantua V. Precision psychiatry roadmap: towards a biology-informed framework for mental disorders. Mol Psychiatry. 2025 Aug;30(8):3846-3855. doi: 10.1038/s41380-025-03070-5 IF: 10.1 Q1 . Epub 2025 Jun 19. PMID: 40533548 IF: 10.1 Q1 ; PMCID: PMC12240818 IF: 10.1 Q1 .