Highlight
This extensive 38-year prospective cohort study from Southern Norway reveals that isolated polymyalgia rheumatica (PMR) does not increase all-cause mortality compared to the general population. Notably, men with PMR exhibited a lower mortality risk than matched controls.
These findings provide vital long-term prognostic reassurance for patients and clinicians managing PMR and biopsy-proven giant cell arteritis (GCA).
Clinical Background and Disease Burden
Polymyalgia rheumatica (PMR) is a common inflammatory rheumatic condition predominantly affecting adults over 50 years, characterized by proximal muscle pain and stiffness. It is often treated with corticosteroids and has an established association with giant cell arteritis (GCA), a systemic vasculitis. Despite its prevalence, robust epidemiological data on the long-term mortality impact of isolated PMR remain scarce, leading to uncertainty in patient prognostication and management.
Clarifying whether PMR independently influences survival is important given the disease’s inflammatory nature, potential treatment-related risks, and overlap with GCA, which has variable mortality outcomes.
Research Methodology
This study utilized a prospective, population-based inception cohort from Aust-Agder County, Norway, including 337 incident cases of PMR and biopsy-confirmed GCA diagnosed between 1987 and 1997. PMR cases met Bird’s criteria and were clinically ascertained by rheumatologists. Patients were followed until death or study end (December 31, 2024), resulting in a maximum follow-up of 35.3 years.
Each patient was matched by age, gender, and residency with 15 population comparators drawn from Norwegian registries. Mortality was assessed using standard mortality ratios (SMRs) with 95% confidence intervals (CIs) and survival analyses via the Kaplan-Meier method with Log-Rank tests.
Key Findings
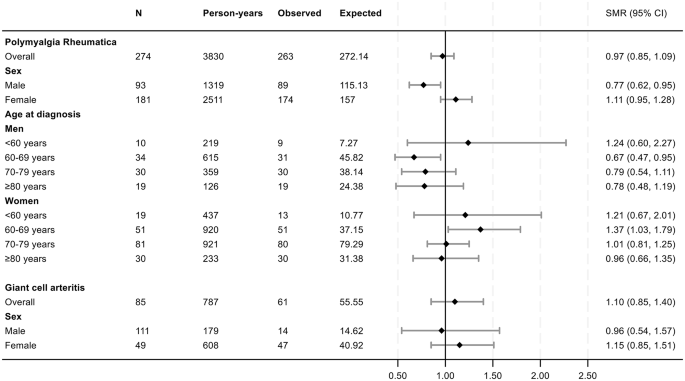
Among 274 isolated PMR patients (mean age 71.9 years, 66.1% female), 96% had died by study end. The overall SMR for PMR was 0.97 (95% CI 0.85–1.09), indicating mortality comparable to the general population. Females had an SMR of 1.11 (95% CI 0.95–1.28), while males demonstrated a significantly lower SMR of 0.77 (95% CI 0.62–0.95), suggesting reduced mortality risk.
Cumulative survival curves showed no significant difference between PMR patients and matched controls (Log-Rank P=0.91). For the 63 GCA patients, overall SMR was 1.10 (95% CI 0.85–1.40), with no significant survival difference compared to controls (Log-Rank P=0.28).
These results collectively indicate that isolated PMR does not increase all-cause mortality risk and that men with PMR may have a survival advantage.
Fig. 2
Forest plot of SMRs for new-onset PMR or GCA compared with the matched comparators. Abbreviations: SMR: standard mortality ratios; N: number of patients; Observed: number of deaths in the PMR and GCA patient cohorts; Expected: number of expected deaths estimated from the total number of deaths observed in the age-, gender and residency-matched population comparator group
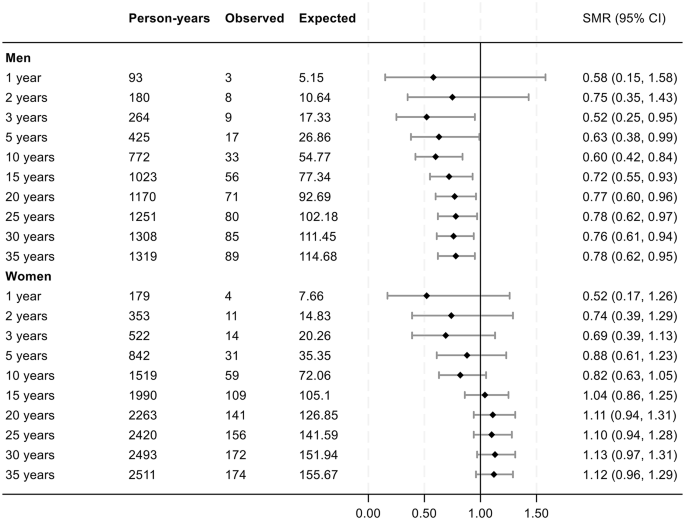
Fig. 3
Forest plot of SMRs across the observation period in the prospective PMR cohort. Data are expressed as years of follow-up from diagnosis of PMR. Abbreviations: SMR: standard mortality ratios; N: number of patients; Observed: cumulative number of deaths in the PMR patient cohort at the defined follow-up times. Expected: cumulative number of expected deaths in the in age-, gender and residency-matched population comparator group, estimated from total number of deaths observed in this group at the different lengths of follow-up
Controversies and Limitations
While the study’s prospective design, large inception cohort, and long follow-up are strengths, limitations include potential changes in diagnostic criteria and treatment approaches over the decades. The cohort is from a single Norwegian county, which may affect generalizability to more ethnically or geographically diverse populations.
Additionally, cause-specific mortality was not detailed, and the impact of comorbidities or corticosteroid adverse effects on survival was not dissected, warranting further research.
Conclusion
This landmark prospective study provides compelling evidence that isolated PMR does not adversely impact long-term survival and offers reassurance to patients and clinicians regarding its prognosis. The observed lower mortality in men with PMR invites additional investigation into sex-specific disease mechanisms and outcomes.
These findings support current clinical practice focusing on symptom control and corticosteroid tapering without heightened concern for increased mortality solely due to PMR.
References
Tengesdal S, Molberg Ø, Holme Ø, Gran JT, Myklebust G. Mortality in polymyalgia rheumatica: a 38-year prospective population-based cohort study from Southern Norway. Arthritis Res Ther. 2025 Jul 21;27(1):154. doi: 10.1186/s13075-025-03613-9 IF: 4.6 Q1