Highlight
1. PIEZO1, a mechanosensitive ion channel, is overexpressed in endothelial cells of type 2 hereditary hemorrhagic telangiectasia (HHT) lesions.
2. Genetic deletion and pharmacological inhibition of PIEZO1 reduce arteriovenous malformation (AVM) formation in Alk1 knockout mouse models.
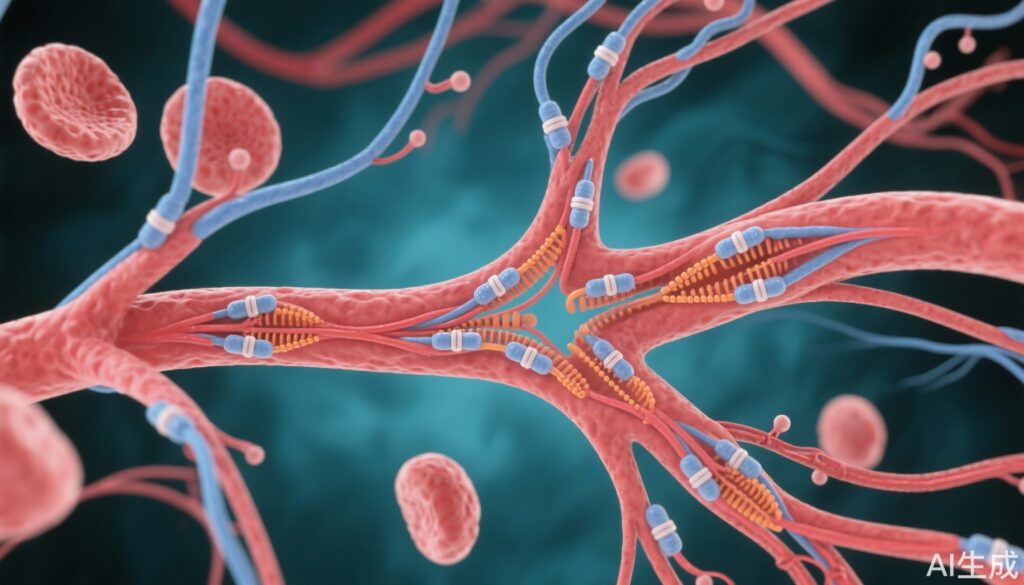
3. PIEZO1 signaling modulates key downstream pathways including VEGFR2/AKT, ERK5-p62-KLF4, and endothelial nitric oxide synthase, attenuating hypoxia, inflammation, and endothelial proliferation.
4. Targeting PIEZO1 presents a promising therapeutic strategy for preventing AVMs in ALK1-related vascular diseases.
Study Background and Disease Burden
Hereditary hemorrhagic telangiectasia (HHT) is a rare but potentially debilitating inherited vascular disorder characterized by the development of arteriovenous malformations (AVMs). AVMs are abnormal direct connections between arteries and veins that bypass capillary beds, leading to increased risks of hemorrhage, ischemia, and high-output heart failure. Type 2 HHT is primarily caused by loss-of-function mutations in the activin receptor-like kinase 1 (ALK1) gene, a receptor involved in transforming growth factor-beta (TGF-β) signaling that critically regulates angiogenesis and vascular remodeling. Currently, treatment options for HHT-related AVMs are limited, largely focusing on symptomatic management or invasive interventions, with no disease-specific molecular therapies available.
The development of AVMs involves complex signaling crosstalk, including overactivation of vascular endothelial growth factor receptor 2 (VEGFR2)-phosphoinositide 3-kinase (PI3K)/AKT pathways in ALK1 deficiency. Yet, the complete spectrum of molecular alterations driving vascular malformations remains incompletely understood. This knowledge gap hinders the discovery of targeted therapies that could prevent or reverse AVM development. The study by Park et al. (2025) leverages cutting-edge single-cell RNA sequencing and mechanistic experiments to uncover novel mediators of AVM pathogenesis, focusing on the mechanosensitive ion channel PIEZO1 and its role in modulating endothelial responses to shear stress in ALK1-deficient vessels.
Study Design
This investigation deployed a robust experimental framework using endothelial cell-specific Alk1 knockout mice to model type 2 HHT. Single-cell RNA sequencing was utilized to profile endothelial cell transcriptomes from retinas of Alk1-deficient and control mice, enabling the identification of cell clusters with abnormal arterio-venous identity and signaling pathways. Expression of PIEZO1 in human and mouse HHT lesions was confirmed using molecular analyses.
To test causality and therapeutic potential, genetic deletion of Piezo1 was performed in Alk1 knockout mice. Pharmacological inhibition using selective PIEZO1 blockers was also assessed for efficacy in reducing AVM formation. Comprehensive evaluation of downstream signaling cascades including VEGFR2/AKT, ERK5-p62-KLF4, and endothelial nitric oxide synthase (eNOS), as well as markers of hypoxia, inflammation, and cellular proliferation, was conducted to elucidate mechanistic pathways.
Key Findings
Analysis revealed a distinct cluster of Alk1 mutant endothelial cells characterized by dysregulated arterio-venous identity and marked overexpression of genes related to fluid shear stress response, hypoxia, inflammation, cell cycle progression, and VEGFR2/PI3K/AKT signaling. Notably, PIEZO1, a mechanosensitive ion channel known to mediate endothelial responses to mechanical forces, was significantly upregulated in these cells as well as in HHT lesions from patients, implicating it as a key effector in AVM pathogenesis.
Functionally, genetic deletion of Piezo1 in Alk1-deficient mice led to a substantial reduction in AVM incidence and size, demonstrating the channel’s causal role. Complementary pharmacological inhibition recapitulated these protective effects. Conversely, overexpression of Piezo1 exacerbated AVM formation induced by ALK1 ligand blockade, reinforcing the pathogenic role of heightened PIEZO1 activity.
Mechanistic studies showed that PIEZO1 inhibition normalized elevated VEGFR2/AKT signaling, attenuated ERK5-p62-KLF4 pathway activation (linked to endothelial plasticity and inflammation), and reduced eNOS overactivity. These changes collectively diminished hypoxia, endothelial proliferation, and inflammatory responses in ALK1-deficient vessels, all key contributors to aberrant vascular remodeling and AVM formation.
Expert Commentary
The study elegantly integrates molecular and physiological data to reveal PIEZO1’s central role as a mechanotransducer in ALK1-related vascular pathology. It extends the understanding of AVM development beyond canonical angiogenic signals by implicating shear stress-mediated ion channel signaling. This is particularly relevant given the dynamic mechanical environment of blood vessels and the known sensitivity of endothelial cells to flow alterations.
While these findings are promising, clinical translation requires cautious consideration. The specificity and safety profile of PIEZO1 inhibitors in humans remain to be established, and the potential systemic effects of modulating mechanotransduction pathways warrant thorough investigation. Moreover, interspecies differences between murine models and humans call for confirmation of results in clinical samples and eventual clinical trials.
Importantly, this research opens avenues for personalized medicine approaches in HHT, identifying patient subsets with high PIEZO1 expression who may benefit most from targeted therapies. Integration with current understanding of TGF-β pathway disruptions in HHT can further refine therapeutic strategies.
Conclusion
The evidence presented by Park et al. identifies PIEZO1 overexpression as a novel molecular driver of AVM formation in type 2 hereditary hemorrhagic telangiectasia. Targeting PIEZO1 signaling mitigates aberrant endothelial responses linked to ALK1 deficiency, offering a promising therapeutic target to prevent or limit vascular malformations. This work advances the mechanistic understanding of HHT pathogenesis and highlights the potential for new, more effective pharmacological interventions to address a critical unmet need in vascular medicine.
Further research is needed to validate these findings clinically and develop safe PIEZO1-targeted therapies suitable for patient use. Nonetheless, this study marks a significant step forward in decoding the complex biology of AVMs and translating molecular insights into clinical benefit for HHT patients.
References
- Park H, Lee S, Furtado J, Robinson M, Antaya RJ, Oh SP, Hong YK, Schwartz MA, Young LH, Eichmann A. PIEZO1 Overexpression in Hereditary Hemorrhagic Telangiectasia Arteriovenous Malformations. Circulation. 2025 Sep 2;152(9):599-615. doi: 10.1161/CIRCULATIONAHA.124.073630. Epub 2025 Jul 16. PMID: 40665909; PMCID: PMC12270330.
- McAllister KA, Grogg KM, Johnson DW, Gallione CJ, Baldwin MA, Jackson CE, et al. Endoglin, a TGF-β binding protein of endothelial cells, is the gene for hereditary hemorrhagic telangiectasia type 1. Nat Genet. 1994 Jul;8(4):345-51.
- Oh SP, Seki T, Goss KA, Imamura T, Yi Y, Donahoe PK, et al. Activin receptor-like kinase 1 modulates transforming growth factor-β 1 signaling in the regulation of angiogenesis. Proc Natl Acad Sci U S A. 2000 Sep 26;97(20):2626-31.
- Li J, Hou B, Tumova S, Muraki K, Bruns A, Ludlow MJ, et al. Piezo1 integration of vascular architecture with physiological force. Nature. 2014 Mar 6;515(7526):279-82.